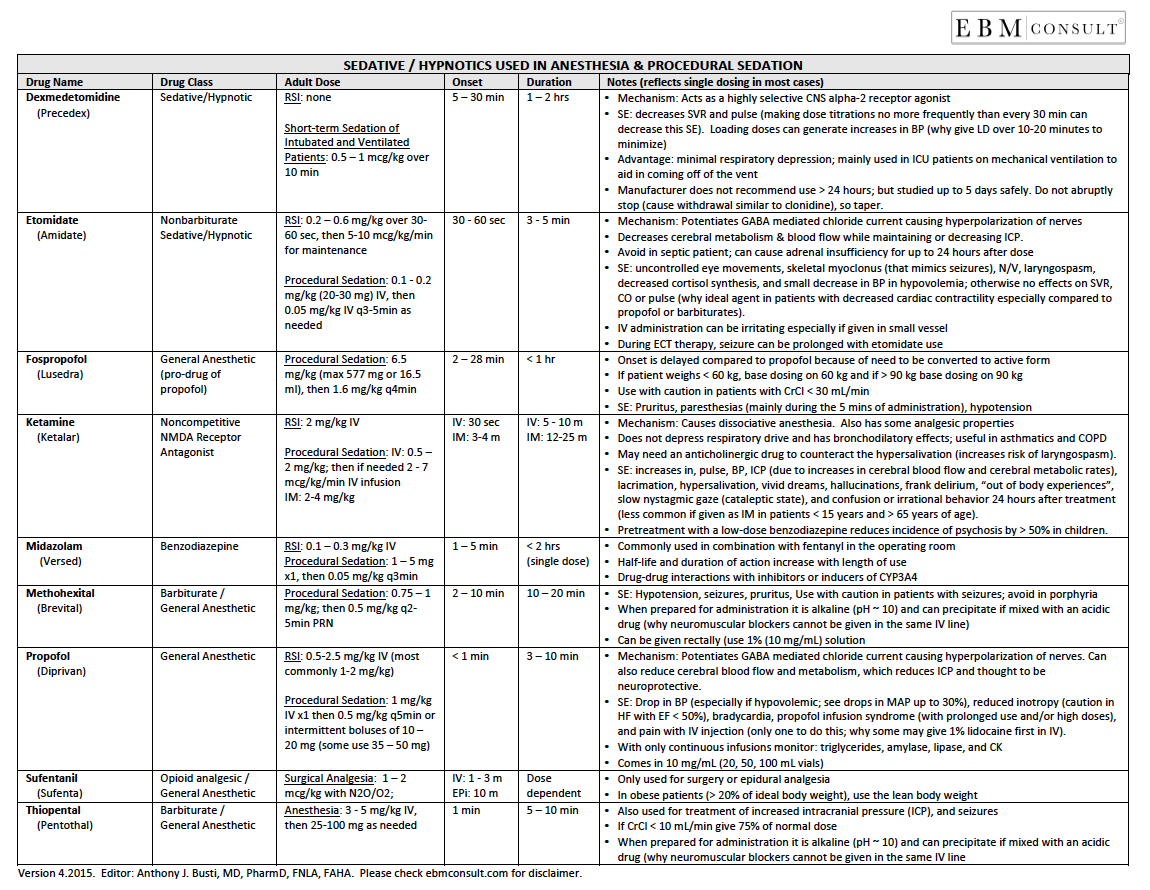
Sedative Hypnotics Medications Used in Anesthesia and Procedural Sedation
- There are a number sedative and hypnotic medications that are commonly used in anesthesia and acute care settings where procedural sedation sometimes is needed.
- A concise review of the content available in the downloadable reference tool is available below.
- The tool was designed to be a quick summary of key points regarding the most commonly used sedative hypnotic agents and is not meant to be exhaustive for every situation.
- To download the PDF file click here
Editor-in-Chief: Anthony J. Busti, MD, PharmD, FNLA, FAHA
Last Reviewed: August 2017
Sedative Hypnotic Reference Tool
|
|---|
- Download this reference tool on sedative hypnotics by click on the image or document icon to the right.
- You may download and share this page or file with others who you think might also benefit.
- Drug Class: Sedative/Hypnotic; Centrally-Acting Alpha-2 Agonist
- Dosing for Short-Term Sedation for Mechanical Ventilation:
- 0.5 - 1 mcg/kg over 10 min, then 0.2 - 0.7 mcg/kg/hr IV infusions
- Dosing in RSI:
- None
- Onset of Action: 5 - 10 min (up to 30 min for peak)
- Duration of Action: 1 - 2 hrs
- Notes:
-
Mechanism of Action: Acts as a highly selective CNS alpha-2 receptor agonist.
-
Side Effects: Decreases SVR and pulse (making dose titrations no more frequently than every 30 min can decrease this side effect). Loading doses can generate increases in BP (giving the loading dose over 10 - 20 min can minimize this unexpected change in BP).
-
Advantages: Minimal respiratory depression; mainly used in ICU patients on mechanical ventilation to aid in coming off of mechanical ventilation.
-
Manufacturer does not recommend use > 24 hours; but studied up to 5 days safely. Do not abruptly stop (cause withdrawal similar to clonidine), so taper.
- Drug Class: Nonbarbiturate; Sedative/Hypnotic
- Dosing for RSI:
- 0.2 - 0.6 mg/kg IV over 30-60 sec, then 5 - 20 mcg/kg/min for maintenance
- Dosing for Procedural Sedation:
- 0.1 - 0.2 mg/kg IV then 0.05 mg/kg IV every 3 - 5 min as needed
- Onset of Action: 30 - 60 sec
- Duration of Action: 3 - 5 min
- Notes:
- Mechanism of Action: Potentiates GABA mediated chloride current causing hyperpolarization of nerves.
- Decreases cerebral metabolism & blood flow while maintaining or decreasing ICP.
- Avoid in septic patient; can cause adrenal insufficiency for up to 24 hours after dose.
- Side Effects: uncontrolled eye movements, skeletal myoclonus (that mimics seizures), N/V, laryngospasm, decreased cortisol synthesis, and small decrease in BP in hypovolemia; otherwise no effects on SVR, CO or pulse (why ideal agent in patients with decreased cardiac contractility especially compared to propofol or barbiturates).
- IV administration can be irritating especially if given in small vessel.
- During electroconvulsive therapy (ECT) therapy, seizure can be prolonged with etomidate use.
- Drug Class: General Anesthetic (pro-drug of propofol)
- Dosing for Procedural Sedation:
- 6.5 mg/kg (max 577 mg or 16.5 mL, then 1.6 mg/kg every 4 mins
- Onset of Action: 2 - 28 min
- Duration of Action: < 1 hr
- Notes:
- Availability has varied over time.
- Onset is delayed compared to propofol because of need to be converted to active form
- If patient weighs < 60 kg, base dosing on 60 kg and if > 90 kg base dosing on 90 kg
- Use with caution in patients with CrCl < 30 mL/min
- Side Effects: Pruritus, paresthesias (mainly during the 5 mins of administration), hypotension
- Drug Class: Noncompetitive NMDA Receptor Antagonist
- Dosing in RSI:
- 2 mg/kg IV x 1
- Dosing for Procedural Sedation:
- IV: 0.5 - 2 mg/kg IV x 1, then if needed 2 - 7 mcg/kg/min IV infusions. (note: some clinicians will administer 1 mg/kg IV over 30 - 60 sec)
- IM: 2 - 4 mg/kg IM x 1 (note: IV preferred route of administration)
- Onset of Action: 1v = 30 sec; IM = 3 - 4 min
- Duration of Action: IV = 5 - 10 min; IM = 12 - 25 min
- Half-life: alpha = 10 - 15 min, beta: 2.5 hrs
- Notes:
- Mechanism of Action: Causes dissociative anesthesia through a direct action on the limbic system. Also has some analgesic properties, which makes it different from other sedative agents.
- Does not depress respiratory drive and has bronchodilatory effects; useful in asthmatics and COPD.
- May need an anticholinergic drug to counteract the hypersalivation (increases risk of laryngospasm).
- Side Effects: increases in pulse, BP, ICP (due to increases in cerebral blood flow and cerebral metabolic rates), lacrimation, hypersalivation, vivid dreams, hallucinations, frank delirium, "out of body experiences", slow nystagmic gaze (cataleptic state), and confusion or irrational behavior 24 hours after treatment (less common if given as IM in patients < 15 years and > 65 years of age). Pretreatment with a low-dose benzodiazepine reduces incidence of psychosis by > 50% in children.
- Drug Class: Benzodiazepine
- Dosing for RSI:
- 0.1 - 0.3 mg/kg IV x 1
- Dosing for Procedural Sedation:
- 1 - 5 mg x 1, then 0.5 mg/kg every 3 min as needed
- Onset of Action: 1 - 5 min
- Duration of Action: < 2 hrs (for single doses)
- Notes:
- Commonly used in combination with fentanyl in the operating room
- Half-life and duration of action increase with length of use
- Drug-drug interactions with inhibitors or
inducers of CYP3A4
- Drug Class: Barbiturate; General Anesthetic
- Dosing for Procedural Sedation:
- 0.75 - 1 mg/kg IV x 1, then 0.5 mg/kg IV every 2 - 5 min as needed
- Onset of Action: 2 - 10 min
- Duration of Action: 10 - 20 min
- Notes:
-
Side Effects: Hypotension, seizures, pruritus, Use with caution in patients with seizures; avoid in porphyria
-
When prepared for administration it is alkaline (pH ~ 10) and can precipitate if mixed with an acidic drug (why neuromuscular blockers cannot be given in the same IV line)
-
Can be given rectally (use 1% (10 mg/mL) solution
- Drug Class: General Anesthetic
- Dosing for RSI:
- 0.5 - 2.5 mg/kg IV x 1 (most common dose is 1 - 2 mg/kg)
- Dosing for Procedural Sedation:
- 1 mg/kg IV x 1, then 0.5 mg/kg every 2 - 5 min as needed. (Note: depending on the clinical scenario and patient's condition, some clinicians will give 50% of the initial loading dose first and if additional sedation is needed they will give the remaining amount 2 - 5 min after that).
- Onset of Action: < 1 min
- Duration of Action: 3 - 10 min
- Notes:
- Mechanism of Action: Potentiates GABA by way of increasing chloride current thereby causing hyperpolarization of nerves. Can also reduce cerebral blood flow and metabolism, which reduces intracranial pressure (ICP) and is thought to be neuroprotective.
- Side Effects: Reduction in BPBP (especially if hypovolemic; see drops in MAP up to 30%), reduced inotropy (caution in HF with EF < 50%), bradycardia, propofol infusion syndrome (with prolonged use and/or high doses), and pain with IV injection (only one to do this; why some may give 1% lidocaine first in IV).
- For Continuous Infusions Monitor: Triglycerides, amylase, lipase, and CK
- Dosage Formulations: Comes in 10 mg/mL (20, 50, 100 mL vials)
- Drug Class: Opioid Analgesic; General Anesthetic
- Dosing for Surgical Anesthesia:
- 1 - 2 mg/kg with N2O/O2
- Onset of Action: 1 - 3 min
- Duration of Action: Dose dependent
- Notes:
- Only used for surgery or epidural analgesia
- In obese patients (> 20% of ideal body weight), use the lean body weight
- Drug Class: Barbiturate; General Anesthetic
- Dosing in Anesthesia:
- 3 - 5 mg/kg IV, then 25 -100 mg as needed
- Onset of Action: 1 min
- Duration of Action: 5 - 10 min
- Notes:
- Also used for treatment of increased intracranial pressure (ICP), and seizures
- If CrCl < 10 mL/min give 75% of normal dose
-
When prepared for administration it is alkaline (pH ~ 10) and can precipitate if mixed with an acidic drug (why neuromuscular blockers cannot be given in the same IV line
- Reference Tool: Neuromuscular Blockers (Paralytics)
- Reference Tool: Antiarrhythmic Drug Table
- Pharmacology: Etomidate's Impact on Adrenal Function