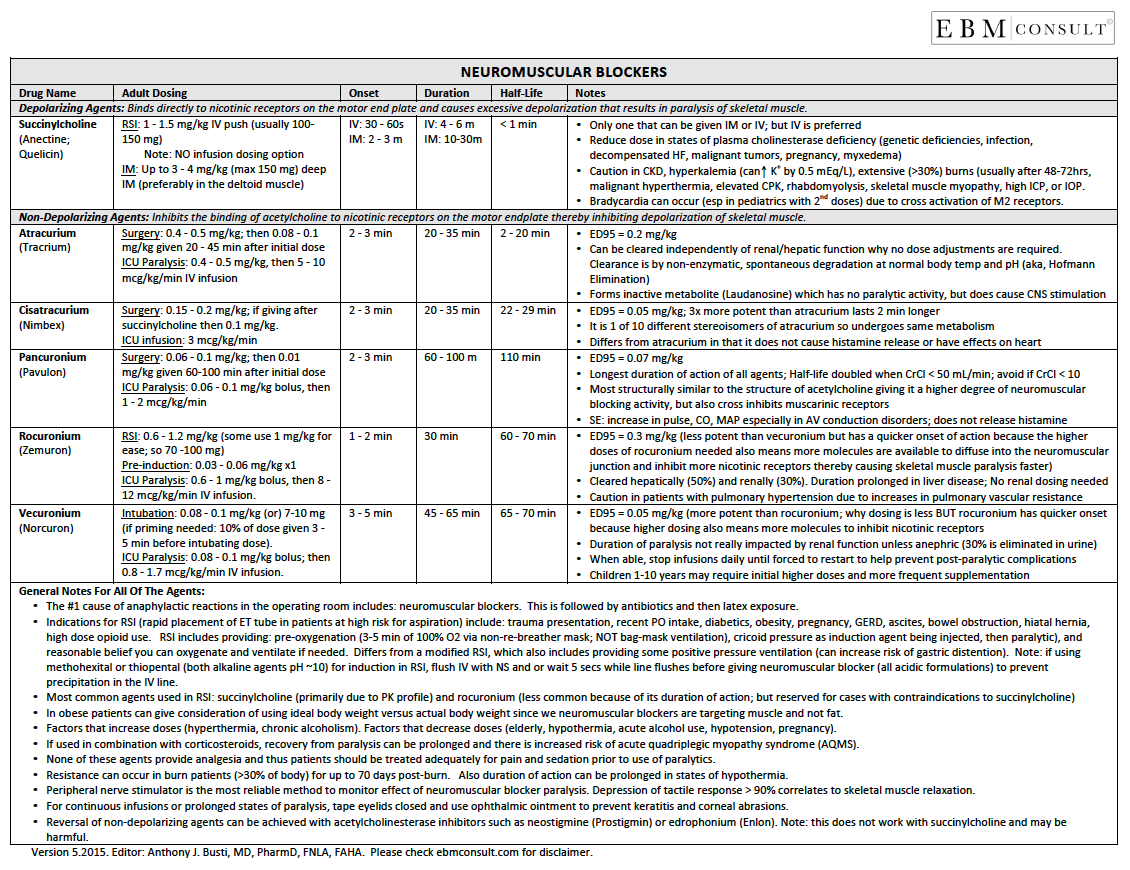
Neuromuscular Blockers: Reference Tool
- Neuromuscular blockers are broken down into 2 main categories, which include depolarizing and non-depolarizing agents.
- A concise review of the content available in the downloadable reference tool is available below.
- The tool was designed to be a quick summary of key points regarding the most commonly used neuromuscular blockers and is not meant to be exhaustive for every situation.
- To download the PDF file Click Here
Editor-in-Chief:
Anthony J. Busti, MD, PharmD, FNLA, FAHA
Last Reviewed: December 2017
Neuromuscular Blockers: Reference Tool
|
|---|
- Download this reference tool on neuromuscular blockers (version 6.2015) by clicking on the image or document icon to the right.
- You may download and share this page or file with others who you think might also benefit from it.
- Succinylcholine (Anectine; Quelicin)
- Dosing for RSI:
- IV: 1 - 1.5 mg/kg IV push (average adult dose is 100 - 150 mg x1).
- IM: 3 - 4 mg/kg IM (max dose of 150 mg; deltoid muscle preferable)
- Onset of Action: IV = 30-60 sec; IM = 2-3 min
- Duration of Action: IV = 4-6 min; IM = 10-30 min
- Half-life: < 1 min
- Notes:
- Only neuromuscular blocking agent that can be given intramuscular (IM)
- Caution in chronic kidney disease (CKD) where hyperkalemia is common, extensive (> 30%) burns that are> 48 hrs old, malignant hyperthermia, elevated CPK, rhabdomyolysis, skeletal muscle myopathy, high intracranial pressure (ICP) or intraocular pressure (IOP)
- Reduce dose in states of plasma cholinesterase deficiency (known genetic deficiencies, infection, decompensated heart failure, malignant tumors, pregnancy, myxedema coma)
- Atracurium (Tracrium)
- Dosing for ICU Paralysis:
- 0.4 - 0.5 mg/kg IV x 1, then 5 - 10 mcg/kg/min IV infusion
- Dosing in Surgery:
- 0.4 - 0.5 mg/kg IV x 1, then 0.08 - 0.1 mcg/kg/min IV given 20 - 45 min after initial dose
- Onset of Action: 2 - 3 min
- Duration of Action: 20 - 35 min
- Half-life: 2 - 20 min
- Notes:
- ED95 = 0.2 mg/kg (note: the ED95 is the dose needed to reduce the twitch height by 95%)
- Can be cleared independently of renal/hepatic function, which is why no dose adjustments needed. Clearance is by non-enzymatic, spontaneous degradation at normal body temperature and pH (a.k.a., Hoffman Elimination). Forms inactive metabolite (laudanosine) which has no paralytic activity, but does cause CNS stimulation.
- Cisatracurium (Nimbex)
- Dosing in ICU:
- 3 mcg/kg/min IV infusion
- Dosing for Surgery:
- 0.15 - 0.2 mg/kg; if giving after succinylcholine then 0.1 mg/kg
- Onset of Action: 2 - 3 min
- Duration of Action: 20 -35 min
- Half-life: 22 - 29 min
- Notes:
- ED95 = 0.05 mg/kg (note: 3x more potent than atracurium; the ED95 is the dose needed to reduce the twitch height by 95%)
- It is 1 of 10 different stereoisomers of atracurium and thus undergoes the same metabolism
- Differs from atracurium in that it does not cause histamine release or have effects on the heart
- Pancuronium (Pavulon)
- Dosing for ICU Paralysis:
- 0.06 - 0.1 mg/kg IV bolus, then 1 - 2 mcg/kg/min IV infusion
- Dosing in Surgery:
- 0.06 - 0.1 mg/kg; then 0.01 mcg/kg given 60-100 min after initial dose
- Onset of Action: 2 - 3 min
- Duration of Action: 60 - 100 min
- Half-life: 110 min
- Notes:
- ED95 = 0.07 mg/kg (note: the ED95 is the dose needed to reduce the twitch height by 95%)
- Longest duration of action of all agents; half-life is doubled when CrCl < 50 mL/min; avoid if CrCl < 10 mL/min
- Most structurally similar to the structure of acetylcholine giving it a higher degree of neuromuscular blocking activity, but can also cross over and inhibit muscarinic receptors
- Does not cause release histamine
- Side Effects: increase in pulse (due to muscarinic inhibition), cardiac output, MAP especially in AV conduction disorders
- Rocuronium (Zemuron)
- Dosing in RSI:
- 0.6 - 1.2 mg/kg (some people use 1 mg/kg to make it easier to remember)
- Dosing in Pre-Induction:
- 0.03 - 0.06 mg/kg IV x 1 1.5 to 3 min prior to succinylcholine
- Dosing in ICU Paralysis:
- 0.6 - 1 mg/kg IV bolus, then 8 - 12 mcg/kg/min IV infusion (note: adjust dose by 10% increments based on peripheral nerve stimulation response or needed clinical response)
- Onset of Action: 1 - 2 min
- Duration of Action: 30 min
- Half-life: 60 -70 min
- Notes:
- ED95 = 0.3 mg/kg (less potent than vecuronium, but has a quicker onset of action because the higher doses of rocuronium needed also means more molecules of the drug are available to diffuse into the neuromuscular junction and inhibit more nicotinic receptors, thereby causing skeletal muscle paralysis faster).
- Cleared hepatically (50%) and renally (30%), therefore the duration is prolonged in liver disease, but no renal dosing needed.
- Caution in patients with pulmonary hypertension due to increases in pulmonary vascular resistance.
- Vecuronium (Norcuron)
- Dosing for Intubation:
- 0.08 - 0.1 mg/kg (or) 7 - 10 mg IV. If priming needed, 10% of dose given 3-5 min before intubating dose.
- Dosing for ICU Paralysis:
- 0.08 - 0.1 mg/kg IV bolus x 1, then 0.8 - 1.7 mcg/kg/min IV infusion
- Onset of Action: 3 - 5 min
- Duration of Action: 45 - 65 min
- Half-life: 65 - 70 min
- Notes:
- ED95 = 0.05 mg/kg (more potent than rocuronium , why dosing is less however rocuronium; the ED95 is the dose needed to reduce the twitch height by 95%)
- Duration of paralysis not impacted by renal function unless anephric (30% is eliminated in the urine).
- When able, stop infusions daily until forced to restart to help prevent post-paralytic complications.
- Children 1 - 10 yrs old may require initial higher doses and more frequent supplementation.
- The #1 cause of anaphylactic reactions in the operating room includes: neuromuscular blockers. This is followed by antibiotics and then latex exposure.
- Indications for RSI (rapid placement of ET tube in patients at high risk for aspiration) include: trauma presentation, recent PO intake, diabetics, obesity, pregnancy, GERD, ascites, bowel obstruction, hiatal hernia, high dose opioid use. RSI includes providing: pre-oxygenation (3-5 min of 100% O2 via non-re-breather mask; NOT bag-mask ventilation), cricoid pressure as induction agent being injected, then paralytic), and reasonable belief you can oxygenate and ventilate if needed. Differs from a modified RSI, which also includes providing some positive pressure ventilation (can increase risk of gastric distention). Note: if using methohexital or thiopental (both alkaline agents pH ~10) for induction in RSI, flush IV with NS and or wait 5 secs while line flushes before giving neuromuscular blocker (all acidic formulations) to prevent precipitation in the IV line.
- Most common agents used in RSI: succinylcholine (primarily due to PK profile) and rocuronium (less common because of its duration of action; but reserved for cases with contraindications to succinylcholine)
- In obese patients can give consideration of using ideal body weight versus actual body weight since we neuromuscular blockers are targeting muscle and not fat.
- Factors that increase doses (hyperthermia, chronic alcoholism). Factors that decrease doses (elderly, hypothermia, acute alcohol use, hypotension, pregnancy).
- If used in combination with corticosteroids, recovery from paralysis can be prolonged and there is increased risk of acute quadriplegic myopathy syndrome (AQMS).
- None of these agents provide analgesia and thus patients should be treated adequately for pain and sedation prior to use of paralytics.
- Resistance can occur in burn patients (>30% of body) for up to 70 days post-burn. Also duration of action can be prolonged in states of hypothermia.
- Peripheral nerve stimulator is the most reliable method to monitor effect of neuromuscular blocker paralysis. Depression of tactile response > 90% correlates to skeletal muscle relaxation.
- For continuous infusions or prolonged states of
paralysis, tape eyelids closed and use ophthalmic ointment to prevent keratitis
and corneal abrasions.
- Reversal of non-depolarizing agents has historically been achieved with acetylcholinesterase inhibitors such as neostigmine (Prostigmin) or edrophonium (Enlon), however in 2015 approved sugammadex (Bridion) to reverse rocuronium and vecuronium in adults undergoing surgery with most patients recovering within 5 mins through a direct binding to the neuromuscular blocker thereby removing the drug from the NMJ. Anaphylactic reactions have occurred with sugammadex use. Note: None of these reversal agents work with succinylcholine and may be harmful .
- Reference Tool: Sedative / Hypnotic Agents
- Reference Tool: Antiarrhythmic Drug Table
- Pharmacology: Etomidate's Impact on Adrenal Function
PDF File of Reference Tool
Depolarizing Agent
Nondepolarizing Agents
Clinical Pearls for All Neuromuscular Blockers
Related Content