Naloxone (Evzio; Narcan): Drug Monograph
|
|---|
- Opioid overdose
- Reversal of respiratory depression from opioid use
- Opioid-induced pruritus (not FDA approved indication)
- General Notes:
- Approved for IV, IM or SubQ administration, but can also give IO, intranasally, or via endotracheal tube.
- Note: While the least desirable route of administration, if endotracheal administration used, the dose is 2 to 2.5 times the initial IV dose.
- Reversal of respiratory depression by partial agonists or mixed agonists/antagonists (e.g., buprenorphine, pentazocine) may be incomplete or require higher doses of naloxone.
- Opioid Overdose:
- Narcan: o.4 mg - 2 mg IV, IM, IO, SubQ, Intranasally, repeat up until a total dose of 10 mg - if no response consider other diagnosis
- Intranasal Use: Give initial dose of 2 mg that is administered as 1 mg in each nostril using a mucosal atomizer device
- Continuous naloxone infusions: If initial response, additional doses may be needed after 30 - 60 min due to the short duration of naloxone especially in a patient who ingested a larger dose of heroin or opioids or an opioid with a long duration of action (e.g., methadone). If repeated doses required, consider a continuous infusion. If needed, administer 1/2 the initial bolus dose used to get desire response, then start infusion at 2/3 of the initial effective dose at an hourly rate. Adjust dose to desired response.
- Evzio (autoinjector): 0.4 mg IM/SubQ into the anterolateral thigh x 1 (entire contents of autoinjector); repeat every 2 to 3 minutes until EMS arrives
- Reversal of Respiratory Depression from Standard Opioid Use:
- 0.04 to 0.4 mg IV, IM, SubQ over 30 - 60 seconds to improve respiratory rate and ventilation. If no response after a total of 0.8 mg has been given, consider different diagnosis.
- Note: Some clinicians recommend placing 1 mL of 0.4 mg/mL along with 9 mL of normal saline into a 10 mL syringe to create a concentration of 0.04 mg/mL to make it easier to administer at a specific time interval.
- Opioid-Induced Pruritus:
- 0.25 mcg/kg/hr as an IV infusion. Note: monitor pain control to make sure there is no reversal of pain control.
- General Notes:
- Patients under the age of one, the caregiver should pinch the thigh muscle while administering the dose.
- Opioid Overdose:
- Narcan:
- If < 5 yrs of age or £ 20 kg: o.1 mg/kg/dose IV, IM, IO, SubQ up to 2 mg; repeat every 2 to 3 minutes as needed.
- If ³ 5 yrs of age or > 20 kg: 2 mg IV, IM, IO, SubQ; repeat every 2 to 3 minutes as needed
- Continuous naloxone infusions: If initial response, additional doses may be needed after 30 - 60 min due to the short duration of naloxone especially in a patient who ingested a larger dose of heroin or opioids or an opioid with a long duration of action (e.g., methadone). If repeated doses required, consider a continuous infusion. If needed, administer 1/2 the initial bolus dose used to get desire response, then start infusion at 2/3 of the initial effective dose at an hourly rate. Adjust dose to desired response.
- Evzio (autoinjector): o.4 mg) IM/SQ into the anterolateral aspect of the thigh, through clothing if necessary, and seek emergency medical assistance
- Reversal of Respiratory Depression from Standard Opioid Use:
- 0.005 to 0.01 mg/kg/dose IV over 30 - 60 seconds to improve respiratory rate and ventilation.
- Injection: 0.4 mg/0.4 mL (1 ML, 10 mL)
- Autoinjector (Evzio): 0.4 mg/mL (0.4 mL) single dose
- Due to the duration of action, keep the patient under continued surveillance and repeated doses of naloxone should be administered, as necessary, while awaiting emergency medical assistance.
- Other supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
- Reversal of respiratory depression by partial agonists or mixed agonists/antagonists such as buprenorphine and pentazocine, may be incomplete.
- Use in patients who are opioid dependent may precipitate acute abstinence syndrome.
- Patients with pre-existing cardiac disease or patients who have received medications with potential adverse cardiovascular effects should be monitored in an appropriate healthcare setting
- In neonates, opioid withdrawal may be life threatening if not recognized and properly treated.
- Use of naloxone hydrochloride in the post-operative setting:
- Hypotension
- Hypertension
- Ventricular tachycardia and fibrillation
- Dyspnea
- Pulmonary edema
- Cardiac arrest
- Death, coma, and encephalopathy have been reported as sequelae of these events.
- Excessive doses in post-operative patients have resulted in significant reversal of analgesia and have caused agitation.
- Abrupt reversal of opioid effects in persons who were physically dependent on opioids has precipitated signs and symptoms of opioid withdrawal including:
- Body aches
- Fever
- Sweating
- Runny nose
- Sneezing
- Piloerection
- Yawning
- Weakness
- Shivering or trembling
- Nervousness
- Restlessness or irritability
- Diarrhea
- Nausea or vomiting
- Abdominal cramps
- Increased blood pressure
- Tachycardia
- In the neonate, opioid withdrawal signs and symptoms also included:
- Convulsions
- Excessive crying
- Hyperactive reflexes
- Pregnancy: Pregnancy Category B
- Labor and Delivery: None
- Nursing Mothers: It is not known whether naloxone hydrochloride is present in human milk. Exercise caution when administered to a nursing woman.
- Renal Impairment: None
- Hepatic Impairment: None
- Pediatric Patients: The safety and effectiveness (for intramuscular and subcutaneous use) have been established in pediatric patients for known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression. Absorption may be erratic or delayed. In neonates an pediatric patients less than 1 year of age, careful observation of the administration site for evidence of residual needle parts and/or signs of infection is warranted.
- Geriatric Patients: Systemic exposure of naloxone can be higher in geriatric patients due to greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
- It is not known whether naloxone hydrochloride is present in human milk. Exercise caution when administered to a nursing woman.
-
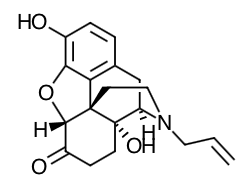
Scientific Name: 17-Allyl-4,5-epoxy-3,14-dihydroxymorphinan-6-one hydrochloride
- Empirical Formula: C19H21NO4 HCl
- Molecular Weight: 363.84
- Antagonizes opioid effects by competing for the same mu-opioid receptor binding sites.
- Reverses the effects of opioids, including respiratory depression, sedation, and hypotension.
- It can also reverse the psychotomimetic and dysphoric effects of agonist-antagonists such as pentazocine.
- Absorption:
- In one pharmacokinetic study in 30 healthy subjects, a single 0.4 mg subcutaneous or intramuscular naloxone injection administered using naloxone provides equivalent naloxone AUC and 15% greater naloxone Cmax in comparison to a single 0.4 mg subcutaneous or intramuscular naloxone injection administered using a standard syringe.
- Following a single injection, the median Tmax of naloxone was reached at 15 minutes (range 5 minutes to 1.2 hours), with a mean (± SD) Cmax value of 1.24 (± 0.64) ng/mL.
- The mean (± SD)
plasma half-life was 1.36 (± 0.32) hours.
- Distribution:
- Following parenteral administration, naloxone is distributed in the body and readily crosses the placenta.
- Plasma protein binding occurs but is relatively weak. Plasma albumin is the major binding constituent but significant binding of naloxone also occurs to plasma constituents other than albumin.
- It is not known whether naloxone is excreted into human milk.
- Metabolism:
- Naloxone hydrochloride is metabolized in the liver, primarily by glucuronide conjugation with naloxone-3-glucoronide as the major metabolite.
- Onset of Action:
- Within 2 minutes, but is shorter when given IV
- Elimination:
- After an oral or intravenous dose, about 25-40% of naloxone is excreted as metabolites in urine within 6 hours, about 50% in 24 hours, and 60-70% in 72 hours.
- Following a single injection, the mean (± SD) plasma half-life of naloxone in healthy adults was 1.28 (± 0.48) hours. In a neonatal study of naloxone injection, the mean (± SD) plasma half-life was observed to be 3.1 (± 0.5) hours.
- Advise the patient and family members or caregivers to read the FDA-approved patient labeling.
- Instruct patients and their family members or caregivers to make sure the medication is present whenever persons may be intentionally or accidentally exposed to an opioid to treat serious opioid overdose (i.e., opioid emergencies).
- Instruct the patients and their family members or caregivers how to recognize the signs and symptoms of an opioid overdose requiring the use of naloxone such as the following:
- Extreme sleepiness - inability to awaken a patient verbally or upon a firm sternal rub.
- Breathing problems - this can range from slow or shallow breathing to no breathing in a patient who cannot be awakened.
- Other signs and symptoms that may accompany sleepiness and breathing problems include the following: extremely small pupils (the black circle in the center of the colored part of the eye) sometimes called "pinpoint pupils", slow heartbeat and/or low blood pressure.
- Instruct them that when in doubt, if a patient is unresponsive, and an opioid overdose is suspected, administer the medication as quickly as possible because prolonged respiratory depression may result in damage to the central nervous system or death.
- Instruct then to seek emergency medical assistance after administering the first dose of naloxone.
- Instruct patients and their family members or caregivers that since the duration of action of most opioids may exceed that of naloxone, seek immediate emergency medical assistance, keep the patient under continued surveillance, and administer repeated doses of naloxone as necessary.
- Instruct patients and their family members or caregivers that the reversal of respiratory depression by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete.
- Instruct patients and their family members or caregivers that the use of naloxone in patients who are opioid dependent may precipitate an acute abstinence syndrome characterized by the following signs and symptoms: body aches, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In neonates, opioid withdrawal may be life threatening if not recognized and properly treated, and may include the following signs and symptoms: convulsions, excessive crying, and hyperactive reflexes.
- Instruct patients and their family members or caregivers about the following important information:
- Naloxone is user actuated and may be administered through clothing (e.g., pants, jeans, etc.) if necessary.
- Inject the drug while pressing into the anterolateral aspect of the thigh. In pediatric patients less than 1 year of age, pinch the thigh muscle while administering.
- Upon actuation, the auto-injector automatically inserts the needle intramuscularly or subcutaneously, delivers the naloxone, and retracts the needle fully into its housing. The needle is not visible before, during, or after injection.
- Each injector can only be used one time.
- If the electronic voice instruction system does not work properly, the injector will still deliver the intended dose of naloxone when used according to the printed instructions on its label.
- The electronic voice instruction are independent of activating the injector and are not required to wait for the voice instructions to be completed prior to moving to the next step in the injection process.
- Post-injection, the black base locks in place, a red indicator appears in the viewing window and electronic visual and audible instructions signal that the intended dose has been delivered.
- The red safety guard should not be replaced under any circumstances. However, the Trainer is designed for re-use and its red safety guard can be removed and replaced.
- It is recommended that patients and caregivers become familiar with the training device provided and read the Instructions for Use; however, untrained caregivers or family members should still attempt to use the injector during a suspected opioid overdose while awaiting definitive emergency medical care.
- Periodically visually inspect the naloxone solution
through the viewing window. If the
solution is discolored, cloudy, or contains solid particles, replace it with a
new injector.
- Replace the medication before its expiration date.
Indications
Dosing
(Adult):
(Pediatrics):
Dosage Forms
Warnings
Adverse Reactions
Special Populations
Breastfeeding
Chemical Structure
Mechanism of Action
Pharmacodynamics
Pharmacokinetics
Counseling Points
Other EBM Related Content
|
|---|
|
MESH Terms & Keywords
|
|---|
|

