Posterior Shoulder Dislocation
Summary:
- Posterior shoulder dislocations are rare compared to anterior shoulder dislocations and occur most commonly from an axial load while the arm is internally rotated and in the adducted position.
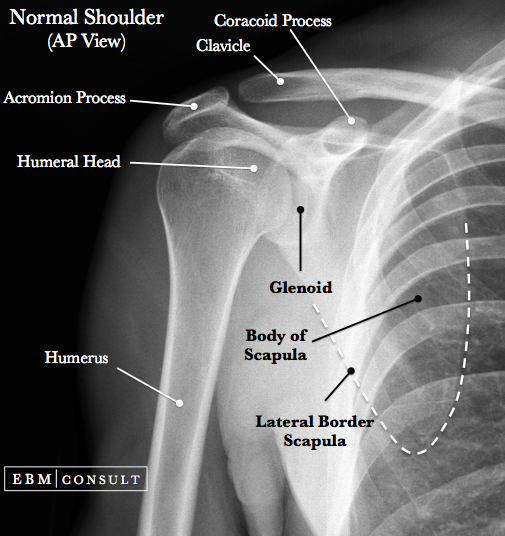
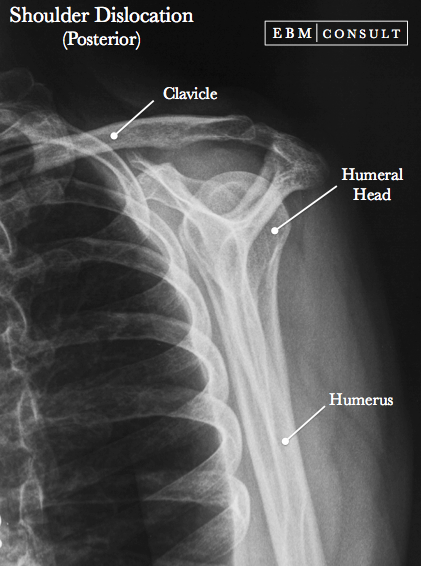
- Initial imaging includes plain radiographs: AP view & axillary view.
- Complications include: Reverse Bankart lesion, Reverse Hill-Sachs lesion, fractures, and recurrent posterior instability.
- Reductions should be done in consultation with orthopedic surgery since some cannot be reduced by closed techniques, but rather need either arthroscopic stabilization or open surgery.
Posterior Shoulder Reduction
|
|---|
-
Less common than anterior dislocations (~ 2% of shoulder dislocations)
-
Patients will commonly present with the arm internally rotated and in the adducted position with resulting pain if attempts to externally rotate or abduct occur
-
Humeral head can be palpated in posterior shoulder just below the acromion process
-
Classically associated with convulsive seizures and electrocution though still uncommon
-
An axial load applied to the arm while it is in an adducted and internally rotated arm where the humeral head is forced posteriorly.
-
The reason that a seizure or electrocution could cause a posterior dislocation has to do with the differing strengths of the rotator cuff muscles (where the internal rotator cuff muscles are stronger than the external muscles and thus a sudden contraction of the internal muscle can cause a dislocation).
- Axillary or Scapular "Y" view:
- The
humeral head will be behind or posterior to the glenoid
- May be helpful in seeing a reverse Hill Sachs lesion
- AP of the Shoulder:
- If there is > 6 mm of space between the anterior rim of glenoid and humeral
head, then highly concerning for a dislocation
- Since the arm is internally rotated the greater tuberosity should be in front of the
humeral head instead of laterally
- AP Shoulder Perpendicular to the Body (not scapula):
- You may see a loss of elliptical overlap since the humeral head would normally overlap the posterior aspect of the glenoid and is now gone
- Reverse Bankart lesion (detachment of the posterior labrum)
- Reverse Hill-Sachs lesion (a defect in the anterior portion of the humeral head produced by the posterior rim of the glenoid; seen on axillary radiographic view
- Lesser tuberosity fracture
- POLPSA lesion (Posterior Labrocapsular
Periosteal Sleeve Avulsion)
- Recurrent posterior instability
-
Check neurovascular status.
-
In many cases the shoulder will reduce on its own, but if not then consult with an orthopedic surgeon prior to reducing as prolonged dislocations (i.e., > 3 weeks as seen in some elderly patients) or the presence of an anterior humeral articular injury are contraindications to doing a closed reduction.
-
Closed reduction technique (if not contraindicated): gentle, prolonged axial traction along the humerus while applying gentle anteriorly directed pressure to get the humeral head over the glenoid rim.
-
If closed reduction is not appropriate for the patient, then orthopedic surgery may consider doing an arthroscopic stabilization procedure or open surgical methods which include: postero-inferior capsular shift, McLaughlin procedure, allograft reconstruction.
-
Once stabilized, consider external rotator cuff muscle strengthening (mainly infraspinatus muscle).
- Kroner K, Lind T, Jensen J.
The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg
1989;108(5):288-90.
- Zhang AL, Montgomery SR, Ngo SS, Hame SL, Wang JC, Gamradt SC. Arthroscopic versus open shoulder stabilization: current practice patterns in the United States. Arthroscopy 2014;30(4):436-43.
Other possible associated injuries include: