Promethazine (Phenergan): Drug Monograph
|
|---|
- Treatment of perennial and seasonal allergic rhinitis, vasomotor rhinitis
- Treatment of allergic conjunctivitis due to inhalant allergens and food
- Treatment of mild, uncomplicated allergic skin manifestations of urticaria and angioedema
- Treatment of amelioration of allergic reactions to blood or plasma
- Treatment of dermographism
- Treatment of anaphylactic reactions, as adjunctive therapy to epinephrine and other standard measures
- Preoperative, postoperative, or obstetric sedation
- Prevention and control of nausea and vomiting associated with certain types of anesthesia and surgery
- Sedation in both children and adults, as well as relief of apprehension and production of light sleep
- Active and prophylactic treatment of motion sickness
- Antiemetic therapy in postoperative patients
- General Notes:
- Can be given orally, rectally, as intramuscular (IM) injection, or intravenously (IV)
- IV administration is generally avoided in the hand and wrist where infiltration into the tissue can result in damage.
- It should be administered slowly over 10 - 15 mins (rate of no more than 25 mg/min).
- IV administration should also be diluted in at least 25 - 50 mL of fluid
- Suppositories are for rectal administration only and should be stored in refrigerator
- Not for subcutaneous administration
- Allergy:
- 25 mg by mouth, rectally, IM or IV at bedtime
- 12.5 mg may be taken before meals and at bedtime, if necessary
- Dosage should be adjusted to the smallest amount adequate to relieve symptoms
- Motion sickness:
- 25 mg by mouth or rectally twice daily
- Take initial dose 1/2 to 1 hour before anticipated travel and repeat 8 to 12 hours later, if necessary
- On succeeding days of travel, take 25 mg upon arising and again before the evening meal
- Nausea and vomiting:
- 25 mg mouth, rectally, IM or IV
- If oral medication cannot be tolerated, give parenterally or by rectal suppository
- 12.5 to 25 mg doses may be repeated, as necessary, at 4 to 6 hour intervals
- Prophylaxis of nausea and vomiting (surgery and postoperative period): 25 mg every 4 to 6 hours, as needed
- Preoperative medication:
- 50 mg rectally, IM or IV with an appropriately reduced dose of narcotic or barbiturate and the required amount of a belladonna alkaloid
- Pre- and Postoperative use:
- 50 mg mouth, rectally, IM or IV the night before surgery to relieve apprehension
- Postoperative sedation and adjunctive use with analgesics:
- 25 -50 mg IM or IV
- Sedation:
- 25-50 mg by tablet or rectal suppository at nighttime, presurgical, or obstetrical sedation
- General Notes:
- Should NOT be used in children under 2 years of age.
- Tablets are not recommended for children under 6 years of age.
- Allergy:
- 25 mg taken at bedtime
- 12.5 mg may be taken before meals and at bedtime, if necessary
- After initial treatment, dosage should be adjusted to the smallest amount adequate to relieve symptoms
- Motion sickness:
- Tablets, syrup, or rectal suppositories: 2.5 to 25 mg, twice daily
- Nausea and vomiting:
- Antiemetics should not be used in vomiting of unknown etiology in children and adolescents
- 0.5 mg/lb.
- Adjust dose to the age and weight of the patient and the severity of the condition being treated
- For preoperative medication:
- 0.25 to 1.1 mg/kg x 1 dose in combination with an appropriately reduced dose of narcotic or barbiturate and the appropriate dose of an atropine-like drug
- Pre- and Postoperative use:
- 12.5-25 mg the night before surgery to relieve apprehension
- Postoperative sedation and adjunctive use with analgesics:
- 12.5 -25 mg IM or IV
- Sedation:
- Oral or rectal suppository: 12.5-25 mg at bedtime
- Tablets: 12.5 mg, 25 mg, 50 mg
- Oral solution: 6.25 mg/5 mL
- Rectal suppositories: 12.5 mg, 25 mg, 50 mg
- Solution for Injection: 25 mg/mL (1 mL), 50 mg/mL (1 mL)
- Promethazine should not be used in pediatric patients less than 2 years of age because of the potential for fatal respiratory depression. Postmarketing cases of respiratory depression, including fatalities, have been reported with use of promethazine in pediatric patients less than 2 years of age. A wide range of weight-based doses of promethazine have resulted in respiratory depression in these patients.
- Caution should be exercised when administering promethazine to pediatric patients 2 years of age and older. It is recommended that the lowest effective dose of promethazine be used in pediatric patients 2 years of age and older and concomitant administration of other drugs with respiratory depressant effects be avoided.
- Known history of hypersensitivity to the drug substance, substances of similar chemical structure or hypersensitivity to the other ingredients
- The sugar free elixir should not be given to patients with allergies to sodium metabisulfite, sodium sulfite or sodium benzoate.
- Newborns or premature infants
- Children under 2 years of age
- Lactating women
- Patients taking monoamine oxidase inhibitors (MAOIs)
- Jaundice induced by other phenothiazine derivatives
- Patients who have received high doses of other CNS depressants and/or are comatose
- Caution is advised in patients with:
- Cardiovascular disease
- Impaired hepatic function
- Renal failure or impairment
- Acute or chronic respiratory impairment
- Epilepsy - may experience increased severity of convulsions
- Hypertensive crisis
- Narrow-angle glaucoma
- Stenosing peptic ulcer
- Symptomatic prostatic hypertrophy
- Bladder neck obstruction
- Pyloroduodenal obstruction
- May cause drowsiness and may increase the effects of alcohol.
- QT interval prolongation
- Solar dermatitis
- Patients with eczema or a tendency to rheumatism
- Bone marrow depression
- Use with caution in patients with bone marrow depression. Leukopenia and agranulocytosis may result
- Neuroleptic malignant syndrome
- Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmias).
- CNS depressive effects - include sedation and impaired performance (impaired driving performance, poor work performance, incoordination, reduced motor skills, and impaired information processing)
- CNS stimulatory effects - may include anxiety, hallucinations, appetite stimulation, muscle dyskinesias and activation of epileptogenic foci
- High doses may cause nervousness, tremor, insomnia, agitation, and irritability.
- Anticholinergic effects - dryness of the eyes, mouth and nose, blurred vision, urinary hesitancy and retention, constipation and tachycardia
- Loss of appetite
- Nausea and vomiting
- Diarrhea
- Restlessness
- Dizziness
- Lassitude
- Incoordination
- Fatigue
- Chief sign is unconsciousness, which is commonly delayed. In addition, convulsions, hallucinations, delirium, acute anxiety, psychotic reactions, extreme hyperaesthesia and hyperalgesia with exterior plantar responses may occur. Anticholinergic action may cause tachycardia flushed skin, dry mouth, and sometimes mydriasis and urinary retention.
- In adults, CNS depression is more common, with drowsiness, coma, and convulsions, progressing to respiratory failure or cardiovascular collapse.
- In infants and children, CNS stimulation predominates over CNS depression, causing ataxia, excitement, tremors, psychoses, hallucinations, convulsions and possibly hyperpyrexia, which may be followed by deepening coma and cardiorespiratory collapse.
- Symptomatic supportive therapy is indicated and maintenance of adequate ventilation should be instituted if necessary.
- Activated charcoal orally or by lavage may be given, or sodium or magnesium sulfate orally as a cathartic.
- Diazepam may be used to control convulsions.
- Acidosis and electrolyte losses should be corrected.
- Avoid analeptics, which may cause convulsions.
- Any depressant effects of promethazine HCL are not reversed by naloxone.
- Epinephrine should not be used, since its use in patients with partial adrenergic blockade may further lower the blood pressure.
- Limited experience with dialysis indicates that it is not helpful.
- CNS depressants (including alcohol, barbiturates, hypnotics, opioid analgesics, anxiolytic sedatives and neuroleptics) - may cause drowsiness and nay enhance the sedative effects of these depressants
- Other antimuscarinic drugs (atropine, tricyclic antidepressants) - have additive antimuscarinic actions
- Monoamine oxidase inhibitors and tricyclic antidepressants (TCAs) - may prolong and intensify the anticholinergic and CNS depressive effects
- Epinephrine - because of the potential for promethazine to reverse epinephrine's vasopressor effect, it should not be used to treat hypotension associated with promethazine overdose.
- Pregnancy: Pregnancy Category C
- Labor and Delivery: May be used alone or as an adjunct to narcotic analgesics during labor. The effect on later growth and development of the newborn is unknown.
- Nursing Mothers: Promethazine is excreted in breast milk; therefore, it should not be used for breastfeeding women.
- Renal Impairment: None
- Hepatic Impairment: None
- Pediatric Patients: May experience paradoxical excitation with promethazine. Should be avoided in children and adolescents with signs and symptoms suggestive of Reye's syndrome. Should not be used in children under 2 years of age, due to the potential for fatal respiratory depression. Caution should be exercised when administering to children, as there is potential for central and obstructive apnoea and reduced arousal. Excessive dosages of antihistamines in children may cause hallucinations, convulsions, and sudden death.
- Geriatric Patients: May experience paradoxical excitation with promethazine. The elderly are more likely to have CNS depressive side effects, including confusion and are more susceptible to the antimuscarinic effects of antihistamines, including hypotension. Dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range. Observe the patient closely.
- Promethazine is excreted in breast milk; therefore, it should not be used for breastfeeding women.
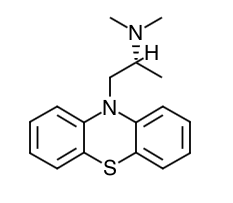
- Scientific Name: 10H-Phenothiazine-10-ethanamine, N,N,α-trimethyl-, monohydrochloride, (±)-
- Empirical Formula: C17H20N2S.HCI
- Molecular Weight: 320.88
- Promethazine, a phenothiazine derivative, is a long acting antihistamine with mild atropine-like anticholinergic effects and some antiserotonin effects, and because of its marked effect on the central nervous system (CNS), it acts as an antiemetic, hypnotic, tranquillizer, and a potentiator of anaesthetics, hypnotics, sedatives and analgesics.
- Inform patients that promethazine may cause marked drowsiness or impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as driving a vehicle or operating machinery.
- Inform patients that the use of alcohol or other central-nervous-system depressants such as sedatives/hypnotics (including barbiturates), narcotics, narcotic analgesics, general anesthetics, tricyclic antidepressants, and tranquilizers, may enhance impairment.
- Inform parents or caregivers of pediatric patients that they should be supervised to avoid potential harm in bike riding or in other hazardous activities.
- Patients should be advised to report any involuntary muscle movements.
- Patients should be advised to avoid prolonged exposure to the sun.
Indications
Dosing (Adult)
Dosing (Pediatric)
Dosage Forms
Black Box Warnings
Contraindications
Warnings
Adverse Reactions
Overdose
Drug Interactions
Special Populations
Breasfeeding
Chemical Structure
Mechanism of Action
Counseling Points
MESH Terms & Keywords
|
|---|
|