Lamotrigine (Lamictal): Drug Monograph
|
|---|
- Epilepsy - adjunctive therapy in patients ≥ 2 years of age, including partial-onset seizures, primary generalized tonic-clonic seizures, and generalized seizures of Lennox-Gastaut syndrome
- Epilepsy - monotherapy in patients ≥ 16 years of age, including partial-onset seizures receiving a single antiepileptic drug (AED) (carbamazepine, phenytoin, phenobarbital, primidone, or valproate)
- Bipolar Disorder in patients ≥ 18 years of age - to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy
- General Dosing & Administration Notes:
- Dosage is based on concomitant medications, indication, and patient age.
- To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded.
- Lamotrigine should be discontinued over a period of at least 2 weeks.
- Chewable tablets: May swallow whole, chewed, or dispersed in water or diluted fruit juice.
- Orally disintegrating tablets: Place onto the tongue and move around in the mouth. Can be swallowed with or without water and taken with or without food
- Bipolar Disorder (patients taking valproate)
- Weeks 1 and 2: 25 mg every other day
- Weeks 3 and 4: 25 mg daily
- Week 5: 50 mg daily
- Week 6 and 7: 100 mg daily
- Bipolar Disorder (for patients NOT taking carbamazepine, phenytoin, phenobarbital, primidone, or valproate):
- Weeks 1 and 2: 25 mg daily
- Weeks 3 and 4: 50 mg daily
- Week 5: 100 mg daily
- Week 6 and 7: 200 mg daily
- Bipolar Disorder (for patients taking carbamazepine, phenytoin, phenobarbital, or primidone and NOT taking valproate):
- Weeks 1 and 2: 50 mg daily
- Weeks 3 and 4: 100 mg daily, in divided doses
- Week 5: 200 mg daily, in divided doses
- Week 6: 300 mg daily, in divided doses
- Week 7: up to 400 mg daily, in divided doses
- Epilepsy (patients taking valproate):
- Weeks 1 and 2: 25 mg every other day
- Weeks 3 and 4: 25 mg every day
- Week 5 onwards to maintenance: Increase by 25 to 50 mg/day every 1 to 2 weeks
- Maintenance: 100-200 mg per day with valproate alone or 100-400 mg per day with valproate and other drugs inducing glucuronidation in 1 or 2 divided doses
- Epilepsy (patients NOT taking carbamazepine, phenytoin, phenobarbital, primidone, or valproate):
- Weeks 1 and 2: 25 mg every day
- Weeks 3 and 4: 50 mg/day
- Week 5 onwards to maintenance: Increase by 50 mg/day every 1 to 2 weeks
- Maintenance: 225-375 mg per day in 2 divided doses
- Epilepsy (patients taking carbamazepine, phenytoin, phenobarbital, or primidone and NOT taking valproate):
- Weeks 1 and 2: 50 mg/day
- Weeks 3 and 4: 100 mg/day, in 2 divided doses
- Week 5 onwards to maintenance: Increase by 100 mg/day every 1 to 2 weeks
- Maintenance: 300-500 mg per day in 2 divided doses
- Conversion from adjunctive therapy --> monotherapy:
- Monotherapy maintenance: 500 mg daily in 2 divided doses
- Conversion from adjunctive therapy with carbamazepine, phenytoin, phenobarbital, or primidone:
- After achieving a dose of 500 mg/day of lamotrigine, withdraw concomitant antiepileptic drug by 20%decrements each week over a 4-week period
- Conversion from adjunctive therapy with valproate:
- Maintain lamotrigine at 200 mg/day and decrease valproate by decrements no >500 mg/day/week to 500 mg/day and then maintain for 1 week
- Increase lamotrigine to 300 mg/day and maintain for 1 week; simultaneously decrease valproate to 250 mg/day and maintain for 1 week
- Increase lamotrigine by 100 mg/day every week to achieve maintenance dose of 500 mg/day; discontinue valproate
- General Dosing & Administration Notes:
- For patients 2-12 years. Only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet. Give in 1-2 divided doses
- Epilepsy (patients taking valproate):
- Weeks 1 and 2: 0.15 mg/kg/day in 1-2 divided doses
- Weeks 3 and 4: 0.3 mg/kg/day in 1-2 divided dosed
- Week 5 onwards to maintenance: Increase every 1-2 weeks by 0.3 mg/kg/day
- Maintenance: 1-5 mg/kg/day (maximum of 200 mg/day) or 1-3 mg/kg/day with valproate alone
- Epileptic (patients NOT taking carbamazepine, phenytoin, phenobarbital, primidone, or valproate):
- Weeks 1 and 2: 0.3 mg/kg/day in 1-2 divided doses
- Weeks 3 and 4: 0.6 mg/kg/day in 2 divided doses
- Week 5 onwards to maintenance: Increase every 1-2 weeks by 0.6 mg/kg/day
- Maintenance: 4.5-7.5 mg/kg/day
- Maximum: 300 mg/day in 2 divided doses
- Epilepsy (patients taking carbamazepine, phenytoin, phenobarbital., or primidone and NOT taking valproate):
- Weeks 1 and 2: 0.6 mg/kg/day in 2 divided doses
- Weeks 3 and 4: 1.2 mg/kg/day in 2 divided doses
- Week 5 onwards to maintenance: Increase every 1-2 weeks by 1.2 mg/kg/day
- Maintenance: 5-15 mg/kg/day
- Maximum: 400 mg/day in 2 divided doses
- Epilepsy (patients > 12 years taking valproate):
- Weeks 1 and 2: 25 mg every other day
- Weeks 3 and 4: 25 mg every day
- Week 5 onward: Increase every 1-2 weeks by 25-50 mg/day
- Maintenance: 100-22 mg/day with valproate alone or 100-400 mg/day with valproate and other drugs inducing glucuronidation in 1 or 2 divided doses
- Epilepsy (patients >12 years not taking carbamazepine, phenytoin, phenobarbital, primidone, or valproate):
- Weeks 1 and 2: 25 mg every day
- Weeks 3 and 4: 50 mg/day
- Week 5 onward: Increase every 1-2 weeks by 50 mg/day
- Maintenance: 225-375 mg/day in 2 divided doses
- Epilepsy (patients >12 years taking carbamazepine, phenytoin, phenobarbital, or primidone, without valproate):
- Weeks 1 and 2: 50 mg/day
- Weeks 3 and 4: 100 mg/day in 2 divided doses
- Weeks 5 onward: Increase every 1-2 weeks by 100 mg/day
- Maintenance: 300-500 mg/day in 2 divided doses
- Significant renal impairment:
- Reduce maintenance doses
- Severe impairment:
- Use with caution
- Moderate/severe without ascites:
- Reduce initial, escalation, and maintenance doses by approximately 25%
- Severe with ascites:
- Reduce initial, escalation, and maintenance doses by 50%
- Adjust maintenance and escalation doses based on clinical response
- Tablets: 25 mg, 100 mg, 150 mg, 200 mg
- Chewable Dispersible Tablets: 2 mg, 5 mg, 25 mg
- Orally Disintegrating Tablets: 25 mg, 50 mg, 100 mg, 200 mg
- Life-threatening serious rashes, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and/or rash-related death. The rate of serious rash is greater in pediatric patients than in adults. Additional factors that may increase the risk of rash include:
- Co-administration with valproate
- Exceeding recommended initial dose of lamotrigine
- Exceeding recommended dose escalation of lamotrigine
- Discontinue at the first sign of rash, unless the rash is clearly not drug related.
-
Life-threatening serious rash and/or rash-related death may result.
-
Fatal or life-threatening hypersensitivity reaction: Multiorgan hypersensitivity reactions, also known as Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), may be fatal or life threatening. Early signs may include rash, fever, and lymphadenopathy. These reactions may be associated with other organ involvement, such as hepatitis, hepatic failure, blood dyscrasias, or acute multiorgan failure. Lamotrigine should be discontinued if alternate etiology for this reaction is not found.
-
Blood dyscrasias (e.g., neutropenia, thrombocytopenia, pancytopenia): May occur, either with or without an associated hypersensitivity syndrome.
-
Suicidal behavior and ideation.
-
Aseptic meningitis reported in pediatric and adult patients.
-
Medication errors involving lamotrigine have occurred. In particular the names LAMICTAL or lamotrigine can be confused with names of other commonly used medications. Medication errors may also occur between the different formulations of lamotrigine.
-
Concomitant use with oral contraceptives
-
Withdrawal seizures
- Adult epilepsy:
- Dizziness
- Headache
- Diplopia
- Ataxia
- Nausea
- Blurred vision
- Somnolence
- Rhinitis
- Rash
- Pediatric epilepsy:
- Vomiting
- Infection
- Fever
- Accidental injury
- Pharyngitis
- Abdominal pain
- Tremor
- Adult bipolar:
- Nausea
- Insomnia
- Somnolence
- Back pain
- Fatigue
- Rash
- Rhinitis
- Abdominal pain
- Xerostomia
- Ataxia, nystagmus, increased seizures, decreased level of consciousness, coma, and intraventricular conduction delay.
- Hospitalization of the patient is advised.
- General supportive care is indicated, including frequent monitoring of vital signs and close observation of the patient.
- Emesis should be induced if indicated.
- Valproate - increases lamotrigine concentrations more than 2-fold.
- Carbamazepine, phenytoin, phenobarbital, and primidone - decrease lamotrigine concentrations by approximately 40%.
- Oral estrogen-containing contraceptives and rifampin - decrease lamotrigine concentrations by approximately 50%.
- Pregnancy: Pregnancy Category C
- Labor and Delivery: The effect is unknown.
- Nursing Mothers: Lamotrigine is present in milk from lactating women. Closely monitor infants for adverse events.
- Renal Impairment: Lamotrigine is metabolized mainly by glucuronic acid conjugation. Reduced maintenance doses may be effective for patients with significant impairment.
- Hepatic Impairment: No dosage adjustments required in patients with mild impairment. With moderate and severe patients: initial, escalation, and maintenance doses should generally be reduced by approximately 25% (without ascites) and 50% (with ascites).
- Pediatric Patients: Indicated for adjunctive therapy in patients ≥ 2 years of age for partial seizures, the generalized seizures of Lennox-Gastaut syndrome, and primary generalized tonic-clonic seizures. Safety and effectiveness in patients below the age of 18 years with Bipolar Disorder have not been established.
- Geriatric Patients: Dose selection should be cautious, usually starting at the low end of the dosing range.
- Lamotrigine is present in milk from lactating women. Closely monitor infants for adverse events.
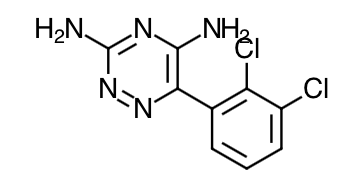
- Scientific Name: 3,5-diamino-6-(2,3-dichlorophenyl)-as-triazine
- Empirical Formula: C9H7N5Cl2
- Molecular Weight: 256.09
- The precise mechanism(s) by which lamotrigine exerts its anticonvulsant action are unknown. In animal models designed to detect anticonvulsant activity, lamotrigine was effective in preventing seizure spread in the maximum electroshock (MES) and pentylenetetrazol (scMet) tests, and prevented seizures in the visually and electrically evoked after-discharge (EEAD) tests for antiepileptic activity. Lamotrigine also displayed inhibitory properties in the kindling model in rats both during kindling development and in the fully kindled state. The relevance of these models to human epilepsy, however, is not known.
- One proposed mechanism of action of lamotrigine, the relevance of which remains to be established in humans, involves an effect on sodium channels. In vitro pharmacological studies suggest that lamotrigine inhibits voltage-sensitive sodium channels, thereby stabilizing neuronal membranes and consequently modulating presynaptic transmitter release of excitatory amino acids (e.g., glutamate and aspartate).
- Although the relevance for human use is unknown, the following data characterize the performance of lamotrigine in receptor binding assays. Lamotrigine had a weak inhibitory effect on the serotonin 5-HT3 receptor (IC50 = 18 µM). It does not exhibit high affinity binding (IC50>100 µM) to the following neurotransmitter receptors: adenosine A1 and A2; adrenergic α1, α2, and β; dopamine D1 and D2; ϒ-aminobutyric acid (GABA) A and B; histamine H1; kappa opioid; muscarinic acetylcholine; and serotonin 5-HT2. Studies have failed to detect an effect of lamotrigine on dihydropyridine-sensitive calcium channels. It had weak effects at sigma opioid receptors (IC 50 = 145 µM). Lamotrigine did not inhibit the uptake of norepinephrine, dopamine, or serotonin (IC 50 >200 µM) when tested in rat synaptosomes and/or human platelets in vitro.
- Folate Metabolism: In vitro, lamotrigine inhibited dihydrofolate reductase, the enzyme that catalyzes the reduction of dihydrofolate to tetrahydrofolate. Inhibition of this enzyme may interfere with the biosynthesis of nucleic acids and proteins. When oral daily doses of lamotrigine were given to pregnant rats during organogenesis, fetal, placental, and maternal folate concentrations were reduced. Significantly reduced concentrations of folate are associated with teratogenesis. Folate concentrations were also reduced in male rats given repeated oral doses of lamotrigine. Reduced concentrations were partially returned to normal when supplemented with folinic acid.
- Accumulation in Kidneys: Lamotrigine accumulated in the kidney of the male rat, causing chronic progressive nephrosis, necrosis, and mineralization. These findings are attributed to α-2 microglobulin, a species- and sex-specific protein that has not been detected in humans or other animal species.
- Melanin Binding: Lamotrigine binds to melanin-containing tissues, e.g., in the eye and pigmented skin. It has been found in the uveal tract up to 52 weeks after a single dose in rodents.
- Cardiovascular: In dogs, lamotrigine is extensively metabolized to a 2-N-methyl metabolite. This metabolite causes dose-dependent prolongations of the PR interval, widening of the QRS complex, and, at higher doses, complete AV conduction block. Similar cardiovascular effects are not anticipated in humans because only trace amounts of the 2-N-methyl metabolite (<0.6% of lamotrigine dose) have been found in human urine. However, it is conceivable that plasma concentrations of this metabolite could be increased in patients with a reduced capacity to glucuronidate lamotrigine (e.g., in patients with liver disease).
- The pharmacokinetics of lamotrigine have been studied in patients with epilepsy, healthy young and elderly volunteers, and volunteers with chronic renal failure.
- Absorption: Lamotrigine is rapidly and completely absorbed after oral administration with negligible first-pass metabolism (absolute bioavailability is 98%). The bioavailability is not affected by food. Peak plasma concentrations occur anywhere from 1.4 to 4.8 hours following drug administration. The lamotrigine chewable/dispersible tablets were found to be equivalent, whether they were administered as dispersed in water, chewed and swallowed, or swallowed as whole, to the lamotrigine compressed tablets in terms of rate and extent of absorption. In terms of rate and extent of absorption, lamotrigine orally disintegrating tablets whether disintegrated in the mouth or swallowed whole with water were equivalent to the lamotrigine compressed tablets swallowed with water.
- Distribution: Estimates of the mean apparent volume of distribution (Vd/F) of lamotrigine following oral administration ranged from 0.9 to 1.3 L/kg. Vd/F is independent of dose and is similar following single and multiple doses in both patients with epilepsy and in healthy volunteers.
- Metabolism: Lamotrigine is metabolized predominantly by glucuronic acid conjugation; the major metabolite is an inactive 2-N-glucuronide conjugate. After oral administration of 240 mg of 14C-lamotrigine (15 μCi) to 6 healthy volunteers, 94% was recovered in the urine and 2% was recovered in the feces. The radioactivity in the urine consisted of unchanged lamotrigine (10%), the 2-N-glucuronide (76%), a 5-N-glucuronide (10%), a 2-N-methyl metabolite (0.14%), and other unidentified minor metabolites (4%).
- Elimination: The elimination half-life and apparent clearance of lamotrigine following administration of LAMICTAL to adult patients with epilepsy and healthy volunteers is summarized in Table 14. Half-life and apparent oral clearance vary depending on concomitant AEDs.
- Drug Interactions: The apparent clearance of lamotrigine is affected by the coadministration of certain medications.
- Estrogen-Containing Oral Contraceptives:
- In 16 female volunteers, an oral contraceptive preparation containing 30 mcg ethinylestradiol and 150 mcg levonorgestrel increased the apparent clearance of lamotrigine (300 mg/day) by approximately 2-fold with mean decreases in AUC of 52% and in Cmax of 39%. In this study, trough serum lamotrigine concentrations gradually increased and were approximately 2-fold higher on average at the end of the week of the inactive hormone preparation compared with trough lamotrigine concentrations at the end of the active hormone cycle.
- Gradual transient increases in lamotrigine plasma levels (approximate 2-fold increase) occurred during the week of inactive hormone preparation ("pill-free" week) for women not also taking a drug that increased the clearance of lamotrigine (carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation. The increase in lamotrigine plasma levels will be greater if the dose of lamotrigine is increased in the few days before or during the "pill-free" week. Increases in lamotrigine plasma levels could result in dose-dependent adverse reactions.
- In the same study, coadministration of lamotrigine (300 mg/day) in 16 female volunteers did not affect the pharmacokinetics of the ethinylestradiol component of the oral contraceptive preparation. There were mean decreases in the AUC and Cmax of the levonorgestrel component of 19% and 12%, respectively. Measurement of serum progesterone indicated that there was no hormonal evidence of ovulation in any of the 16 volunteers, although measurement of serum FSH, LH, and estradiol indicated that there was some loss of suppression of the hypothalamic-pituitary-ovarian axis.
- The effects of doses of lamotrigine other than 300 mg/day have not been systematically evaluated in controlled clinical trials.
- The clinical significance of the observed hormonal changes on ovulatory activity is unknown. However, the possibility of decreased contraceptive efficacy in some patients cannot be excluded. Therefore, patients should be instructed to promptly report changes in their menstrual pattern (e.g., break-through bleeding).
- Dosage adjustments may be necessary for women receiving estrogen-containing oral contraceptive preparations.
- Other Hormonal Contraceptives or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lomotrigine in the presence of progestogens alone will likely not be needed.
- Bupropion: The pharmacokinetics of a 100-mg single dose of lamotrigine in healthy volunteers (n = 12) were not changed by coadministration of bupropion sustained-release formulation (150 mg twice daily) starting 11 days before lamotrigine.
- Carbamazepine: Lamotrigine has no appreciable effect on steady-state carbamazepine plasma concentration. Limited clinical data suggest there is a higher incidence of dizziness, diplopia, ataxia, and blurred vision in patients receiving carbamazepine with lamotrigine than in patients receiving other AEDs with lamotrigine. The mechanism of this interaction is unclear. The effect of lamotrigine on plasma concentrations of carbamazepine-epoxide is unclear. In a small subset of patients (n = 7) studied in a placebo- controlled trial, lamotrigine had no effect on carbamazepine-epoxide plasma concentrations, but in a small, uncontrolled study (n = 9), carbamazepine-epoxide levels increased. The addition of carbamazepine decreases lamotrigine steady-state concentrations by approximately 40%.
- Felbamate: In a study of 21 healthy volunteers, coadministration of felbamate (1,200 mg twice daily) with lamotrigine (100 mg twice daily for 10 days) appeared to have no clinically relevant effects on the pharmacokinetics of lamotrigine.
- Folate Inhibitors: Lamotrigine is a weak inhibitor of dihydrofolate reductase. Prescribers should be aware of this action when prescribing other medications that inhibit folate metabolism.
- Gabapentin: Based on a retrospective analysis of plasma levels in 34 patients who received lamotrigine both with and without gabapentin, gabapentin does not appear to change the apparent clearance of lamotrigine.
- Levetiracetam: Potential drug interactions between levetiracetam and lamotrigine were assessed by evaluating serum concentrations of both agents during placebo-controlled clinical trials. These data indicate that lamotrigine does not influence the pharmacokinetics of levetiracetam and that levetiracetam does not influence the pharmacokinetics of lamotrigine.
- Lithium: The pharmacokinetics of lithium were not altered in healthy subjects (n = 20) by coadministration of lamotrigine (100 mg/day) for 6 days.
- Olanzapine: The AUC and Cmax of olanzapine were similar following the addition of olanzapine (15 mg once daily) to lamotrigine (200 mg once daily) in healthy male volunteers (n=16) compared with the AUC and Cmax in healthy ale volunteers receiving olanzapine alone (n=16). In the same study, the AUC and Cmax of lamotrigine were reduced on average by 24% and 20%, respectively, following the addition of olanzapine to lamotrigine in healthy male volunteers compared with those receiving lamotrigine alone. This reduction in lamotrigine plasma concentrations is not expected to be clinically relevant.
- Oxcarbazepine:
- The AUC and Cmax of oxcarbazepine and its active 10-monohydroxy oxcarbazepine metabolite were not significantly different following the addition of oxcarbazepine (600 mg twice daily) to lamotrigine (200 mg once daily) in healthy male volunteers (n = 13) compared with healthy male volunteers receiving oxcarbazepine alone n=13).
- In the same study, the AUC and Cmax of lamotrigine were similar following the addition of oxcarbazepine (600 mg twice daily) to lamotrigine in healthy male volunteers compared with those receiving lamotrigine alone. Limited clinical data suggest a higher incidence of headache, dizziness, nausea, and somnolence with coadministration of lamotrigine and oxcarbazepine compared with lamotrigine alone or oxcarbazepine alone.
- Phenobarbital, Primidone: The addition of phenobarbital or primidone decreases lamotrigine steady-state concentrations by approximately 40%.
- Phenytoin: Lamotrigine has no appreciable effect on steady-state phenytoin plasma concentrations in patients with epilepsy. The addition of phenytoin decreases lamotrigine steady-state concentrations by approximately 40%.
- Pregabalin: Steady-state trough plasma concentrations of lamotrigine were not affected by concomitant pregabalin (200 mg 3 times daily) administration. There are no pharmacokinetic interactions between lamotrigine and pregabalin.
- Rifampin: In 10 male volunteers, rifampin (600 mg/day for 5 days) significantly increased the apparent clearance of a single 25-mg dose of lamotrigine by approximately 2-fold (AUC decreased by approximately 40%).
- Topiramate: Topiramate resulted in no change in plasma concentrations of lamotrigine. Administration of lamotrigine resulted in a 15% increase in topiramate concentrations.
- Valproate: When lamotrigine was administered to healthy volunteers (n = 18) receiving valproate, the trough steady-state valproate plasma concentrations decreased by an average of 25% over a 3-week period, and then stabilized. However, adding lamotrigine to the existing therapy did not cause a change in valproate plasma concentrations in either adult or pediatric patients in controlled clinical trials. The addition of valproate increased lamotrigine steady-state concentrations in normal volunteers by slightly more than 2-fold. In one study, maximal inhibition of lamotrigine clearance was reached at valproate doses between 250 and 500 mg/day and did not increase as the valproate dose was further increased.
- Zonisamide: In a study of 18 patients with epilepsy, coadministration of zonisamide (200 to 400 mg/day) with lamotrigine (150 to 500 mg/day for 35 days) had no significant effect on the pharmacokinetics of lamotrigine.
- Known Inducers or Inhibitors of Glucuronidation: Drugs other than those listed above have not been systematically evaluated in combination with lamotrigine. Since lamotrigine is metabolized predominately by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
- Other: Results of in vitro experiments suggest that clearance of lamotrigine is unlikely to be reduced by concomitant administration of amitriptyline, clonazepam, clozapine, fluoxetine, haloperidol, lorazepam, phenelzine, risperidone, sertraline, or trazodone. Results of in vitro experiments suggest that lamotrigine does not reduce the clearance of drugs eliminated predominantly by CYP2D6.
- Special Populations:
- Patients With Renal Impairment: Twelve volunteers with chronic renal failure (mean creatinine clearance: 13 mL/min, range: 6 to 23) and another 6 individuals undergoing hemodialysis were each given a single 100-mg dose of lamotrigine. The mean plasma half-lives determined in the study were 42.9 hours (chronic renal failure), 13.0 hours (during hemodialysis), and 57.4 hours (between hemodialysis) compared with 26.2 hours in healthy volunteers. On average, approximately 20% (range: 5.6 to 35.1) of the amount of lamotrigine present in the body was eliminated by hemodialysis during a 4-hour session.
- Hepatic Disease: The pharmacokinetics of lamotrigine following a single 100-mg dose of lamotrigine were evaluated in 24 subjects with mild, moderate, and severe hepatic impairment (Child-Pugh Classification system) and compared with 12 subjects without hepatic impairment. The patients with severe hepatic impairment were without ascites (n = 2) or with ascites (n = 5). The mean apparent clearances of lamotrigine in patients with mild (n = 12), moderate (n = 5), severe without ascites (n = 2), and severe with ascites (n = 5) liver impairment were 0.30 ± 0.09, 0.24 ± 0.1, 0.21 ± 0.04, and 0.15 ± 0.09 mL/min/kg, respectively, as compared with 0.37 ± 0.1 mL/min/kg in the healthy controls. Mean half-lives of lamotrigine in patients with mild, moderate, severe without ascites, and severe with ascites hepatic impairment were 46 ± 20, 72 ± 44, 67 ± 11, and 100 ± 48 hours, respectively, as compared with 33 ± 7 hours in healthy controls.
- Age:
- Pediatric Patients: The pharmacokinetics of lamotrigine following a single 2-mg/kg dose were evaluated in 2 studies of pediatric patients (n = 29 for patients 10 months to 5.9 years of age and n = 26 for patients 5 to 11 years of age). Forty-three patients received concomitant therapy with other AEDs and 12 patients received lamotrigine as monotherapy. Population pharmacokinetic analyses involving patients 2 to 18 years of age demonstrated that lamotrigine clearance was influenced predominantly by total body weight and concurrent AED therapy. The oral clearance of lamotrigine was higher, on a body weight basis, in pediatric patients than in adults. Weight-normalized lamotrigine clearance was higher in those subjects weighing less than 30 kg, compared with those weighing greater than 30 kg. Accordingly, patients weighing less than 30 kg may need an increase of as much as 50% in maintenance doses, based on clinical response, as compared with subjects weighing more than 30 kg being administered the same AEDs. These analyses also revealed that, after accounting for body weight, lamotrigine clearance was not significantly influenced by age. Thus, the same weight-adjusted doses should be administered to children irrespective of differences in age. Concomitant AEDs which influence lamotrigine clearance in adults were found to have similar effects in children.
- Elderly: The pharmacokinetics of lamotrigine following a single 150-mg dose of lamotrigine were evaluated in 12 elderly volunteers between the ages of 65 and 76 years (mean creatinine clearance = 61 mL/min, range: 33 to 108 mL/min). The mean half-life of lamotrigine in these subjects was 31.2 hours (range: 24.5 to 43.4 hours), and the mean clearance was 0.40 mL/min/kg (range: 0.26 to 0.48 mL/min/kg).
- Gender: The clearance of lamotrigine is not affected by gender. However, during dose escalation of lamotrigine in one clinical trial in patients with epilepsy on a stable dose of valproate (n = 77), mean trough lamotrigine concentrations, unadjusted for weight, were 24% to 45% higher (0.3 to 1.7 mcg/mL) in females than in males.
- Race: The apparent oral clearance of lamotrigine was 25% lower in non-Caucasians than Caucasians.
- Patients should be advised to notify their physician if they stop taking lamotrigine for any reason and not to resume without consulting their physician.
- Inform patients that a rash or other signs or symptom of hypersensitivity (e.g., fever, lymphadenopathy) may herald a serious medical event. Patient should report any such occurrence to a physician immediately.
- Patients should be advised that multi-organ hypersensitivity reactions and acute multi-organ failure may occur. Isolated organ failure or isolated blood dyscrasias without evidence of multi-organ hypersensitivity may also occur. Patients should contact their physician immediately if they experience any signs or symptoms of these conditions.
- Lamotrigine may increase the risk of suicidal thoughts and behavior. Patients should be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to health care providers.
- If worsening of seizure control occurs, patients should notify their physician.
- Patients should be advised that lamotrigine may cause dizziness, somnolence, and other symptoms and signs of CNS depression.
- Patients should neither drive a car to operate other complex machinery until they have gained sufficient experience on lamotrigine to gauge whether or not it adversely affects their mental and/or motor performance.
- Patients should be advised to notify their physicians if they become pregnant or intend to become pregnant during therapy, as well if they intend to breastfeed or are breastfeeding an infant. Patients should also be encouraged to enroll in the NAAED Pregnancy Registry if they become pregnant.
- Women should be advised to notify their physician if they plan to start or stop use of oral contraceptives or other female hormonal preparations.
- Women should also be advised to promptly notify their physician if they experience adverse reactions or changes in menstrual pattern.
- Patients should be advised that lamotrigine may cause aseptic meningitis and they should contact their physician if they develop signs and symptoms of meningitis.
- Strongly advise patients to visually inspect tablets to verify if the correct drug/formulation was dispensed each time the prescription is filled.
Indications
Dosing (Adult)
Dosing (Pediatrics)
Renal Dosing
Hepatic Dosing
Dosage Forms
Black Box Warnings
Warnings
Adverse Reactions
Overdose
Drug Interactions
Special Populations
Breasfeeding
Chemical Structure
Mechanism of Action
• Lamotrigine did not inhibit N-methyl d-aspartate (NMDA)-induced depolarizations in rat cortical slices or NMDA-induced cyclic GMP formation in immature rat cerebellum, nor did lamotrigine displace compounds that are either competitive or noncompetitive ligands at this glutamate receptor complex (CNQX, CGS, TCHP). The IC 50 for lamotrigine effects on NMDA-induced currents (in the presence of 3 µM of glycine) in cultured hippocampal neurons exceeded 100 µM.
• The mechanisms by which lamotrigine exerts its therapeutic action in Bipolar Disorder have not been established.
Pharmacodynamics
Pharmacokinetics
Counseling Points
MESH Terms & Keywords
|
|---|
|