Dabigatran (Pradaxa): Drug Monograph
|
|---|
- Deep vein thrombosis (DVT) and pulmonary embolism (PE)
- Reduce the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation
- DVT & PE:
- Treat with parenteral anticoagulant for first 5-10 days, then start dabigatran
- If CrCl > 30 mL/min: 150 mg orally twice daily
- If CrCl 15-30 mL/min: 75 mg orally twice a day
- Stroke Prevention in Non-valvular Atrial Fibrillation:
- 150 mg orally twice a day
- If CrCl > 30 mL/min: 150 mg orally twice daily
- If CrCl 15-30 mL/min: 75 mg orally twice a day
- If switching from parenteral anticoagulant to dabigatran:
- Start dabiatran within 2 hrs
of next dose of parenteral agent
- If switching from dabigatran to a parenteral anticoagulation:
- Start the parenteral
anticoagulant 12 hrs (if CrCl > 30 mL/min) or 24 (if CrCl < 30 mL/min) after
the last dose of dabigatran
- If switching from warfarin to dabigatran:
- Stop warfarin and when INR < 2, start
dabigatran
- If switching from dabigatran to warfarin:
- If CrCl > 50 mL/min start dabigatran 3
days before stopping warfarin;
- If CrCl 31 to 50 mL/min start dabigatran 2 days before stopping warfarin;
- If CrCl 15 to 30 mL/min start warfarin 1 day before
stopping dabigatran; and
- If CrCl < 15 mL/min no official recommendations.
- Pediatric Starting Dose: None
- Renal Dose Adjustment:
- Once the CrCl < 30 mL/min, reduce the dose by at least 50%.
- If CrCl is < 30 mL/min and the patient is on a P-gp inhibitor, then
dabigatran should not be used.
- Hepatic Dosing:
- No dosage adjustments needed in patients with moderate impairment
- Discontinuing dabigatran places patients at an increased risk of thrombotic events and if dabigatran is stopped for something other than pathologic bleeding, consider using another anticoagulant.
- Active pathologic bleeding
- History of serious hypersensitivity reaction to
dabigatran
- Mechanical prosthetic heart valve
- Risk of bleeding
- Bioprosthetic heart valves (dabigatran is not
recommended)
- P-gp inducers and inhibitors
-
No specific antidote exists.
-
Dabigatran can be partially dialyzed (~57% can be removed over 4 hrs) but has limited data.
-
Can consider PCC (prothrombin complex concentrate) though efficacy not established. At least 1 case of reversal using FEIBA NF has been documented.
-
P-gp inducers: rifampin
-
P-gp inhibitors: dronedarone, ketoconazole in patients with CrCl 30-50 mL/min (reduce dose of dabigatran to 75 mg twice a day); if CrCl was also < 30 ml/min then avoid use of dabigatran
-
Pregnancy: Pregnancy category C
-
Labor and Delivery: Safety and effectiveness of dabigatran during labor and delivery have not been studied in clinical trials
-
Nursing Mothers: It is unknown if dabigatran is excreted in human milk
-
Renal Impairment: Reduce the dose once the CrCl < 30 ml/min
-
Hepatic Impairment: Administration in patients with moderate hepatic impairment (Child-Pugh B) showed a large inter-subject variability, but no evidence of a consistent change in exposure or pharmacodynamics
-
Pediatric Patients: Safety and efficacy has not been established in pediatric patients
-
Geriatric Patients: Risk of bleeding increases with age
-
Overdose may lead to hemorrhagic complications.
-
There is no official reversal agent or antidote for dabigatran.
-
Dabigatran is primarily eliminated by the kidneys with a low plasma protein binding of approximately 35%. Hemodialysis can remove dabigatran; however, data supporting this approach are limited. Using a high-flux dialyzer, blood flow rate of 200 mL/min, and dialysate flow rate of 700 mL/min, approximately 49% of total dabigatran can be cleared from plasma over 4 hours. At the same dialysate flow rate, approximately 57% can be cleared using a dialyzer blood flow rate of 300 mL/min, with no appreciable increase in clearance observed at higher blood flow rates. Upon cessation of hemodialysis, a redistribution effect of approximately 7% to 15% is seen.
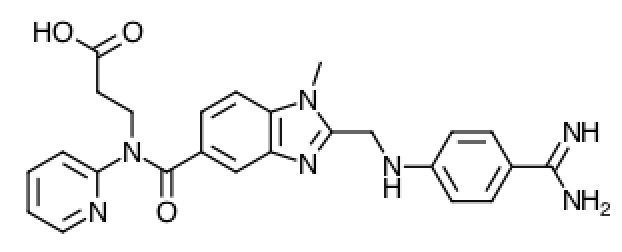
- Dabigatran and its acyl glucuronides are competitive, direct thrombin inhibitors (DTI). Because thrombin (serine protease) enables the conversion of fibrinogen into fibrin during the coagulation cascade, its inhibition prevents the development of a thrombus. Both free and clot-bound thrombin, and thrombin-induced platelet aggregation are inhibited by the active components of dabigatran.
-
Absorption: The absolute bioavailability following oral administration is ~ 3 to 7%. Dabigatran etexilate is a substrate of the efflux cell membrane transporter P-gp. After oral administration in healthy volunteers, the Cmax occurs at 1 hour post-administration in the fasted state. Coadministration of dabigatran with a high-fat meal delays the time to Cmax by approximately 2 hours but has no effect on the bioavailability; Dabigatran can be administered with or without food. The oral bioavailability of dabigatran etexilate increases by 75% when the pellets are taken without the capsule shell compared to the intact capsule formulation. Dabigatran capsules should therefore not be broken, chewed, or opened before administration.
- Distribution: Dabigatran is approximately 35% bound to human plasma proteins. The red blood cell to plasma partitioning of dabigatran measured as total radioactivity is less than 0.3. The volume of distribution of dabigatran is 50 to 70 L. Dabigatran pharmacokinetics are dose proportional after single doses of 10 to 400 mg. Given twice daily, dabigatran's accumulation factor is approximately two
- Metabolism: After oral administration, dabigatran etexilate is converted to dabigatran. The cleavage of the dabigatran etexilate by esterase-catalyzed hydrolysis to the active principal dabigatran is the predominant metabolic reaction. Dabigatran is not a substrate, inhibitor, or inducer of CYP450 enzymes. Dabigatran is subject to conjugation forming pharmacologically active acyl glucuronides. Four positional isomers, 1-O, 2-O, 3-O, and 4-O-acylglucuronide exist, and each accounts for less than 10% of total dabigatran in plasma.
- Elimination: Dabigatran is eliminated primarily in the urine. Renal clearance of dabigatran is 80% of total clearance after intravenous administration. After oral administration of radiolabeled dabigatran, 7% of radioactivity is recovered in urine and 86% in feces. The half-life of dabigatran in healthy subjects is 12 to 17 hours.
- Remind patients not to stop dabigatrain without talking to the health care provider who prescribed it.
- Keep dabigatran in the original bottle and to protect from moisture.
- Do not put dabigatran in pill boxes or pill organizers.
- When more than one bottle is dispensed to the patient, instruct them to open only one bottle at a time.
- Instruct patient to remove only one capsule from the opened bottle at the time of use. The bottle should be immediately and tightly closed.
- Advise patients not to chew or break the capsules before swallowing them and not to open the capsules and take the pellets alone.
- Inform patients that they may bleed more easily, may bleed longer, and should call their health care provider for any signs or symptoms of bleeding.
- Unusual bruising (bruises that appear without known cause or that get bigger)
- Pink or brown urine
- Red or black or "tarry-looking" stools
- Coughing up blood
- Vomiting blood, or vomit that looks like coffee grounds
- Pain, swelling or discomfort in a joint
- Headaches, dizziness, or weakness
- Reoccurring nose bleeds
- Unusual bleeding from gums
- Bleeding from a cut that takes a long time to stop
- Menstrual bleeding or vaginal bleeding that is heavier than normal
- Dyspepsia (upset stomach), burning, or nausea
- Abdominal pain or discomfort
- Epigastric discomfort, GERD (gastric indigestion)
Information for patients:
Bleeding:
Instruct patients to seek emergency care right away if they have any of the following, which may be a sign or symptom of serious bleeding:
Instruct patients to call their health care provider or to get prompt medical attention if they experience any signs or symptoms of bleeding:
Gastrointestinal Adverse Reactions
Instruct patients to call their health care provider if
they experience any signs or symptoms of dyspepsia or gastritis:
Invasive or Surgical Procedures Instruct patients to inform their health care provider that they are taking dabigatran before any invasive procedure (including dental procedures) is scheduled.
Concomitant Medications Ask patients to list all prescription medications, over-the-counter medications, or dietary supplements they are taking or plan to take so their health care provider knows about other treatments that may affect bleeding risk (e.g., aspirin or NSAIDs) or dabigatran exposure (e.g., dronedarone or systemic ketoconazole).
Prosthetic Heart Valves Instruct patients to inform their health care provider if they will have or have had surgery to place a prosthetic heart valve.