Anyone who does a simple literature search will encounter
a plethora of articles discussing, debating, and even arguing over this topic.
The reasons for all of these issues, in our opinion, has to do with numerous
inconsistencies among studies in the doses and duration of ibuprofen used, the
timing of ibuprofen dosing in relation to the administration of aspirin, the
dose and formulation (enteric or non-enteric coated) of aspirin used, the
patient population studied (healthy volunteers vs. patients with known
cardiovascular disease (CVD)), whether surrogate laboratory markers were used
versus tests that actually assess platelet aggregation, and lastly the study
design used by the investigators to generate their findings.1-6 As such,
it is very difficult, to nearly impossible, to extrapolate the current data
from each of these studies, all of which have limitations or inconsistencies
among each other, and generate a definitive answer that can actually translate
into clinically meaningful endpoints that are applicable to the general
population. Some of the discrepancies in the literature may be due to the
ability of platelets to aggregate at times when the concentrations of the
non-steroidal anti-inflammatory drugs (NSAIDs) are low versus early on after
administration when concentrations are higher.7 By the time the ibuprofen
is freed from the binding site in COX-1, some of the aspirin will already have
been eliminated from the body.
The
Food & Drug Administration (FDA) warning to healthcare professionals
recently stated, "Patients who use immediate release aspirin (not enteric
coated) and take a single dose of ibuprofen 400 mg should dose the ibuprofen at
least 30 minutes or longer after aspirin ingestion, or more than 8 hours before
aspirin ingestion to avoid attenuation of aspirin's effect. In addition,
there are a number of studies with conflicting findings."8 Based on
this recommendation, the purpose of this issue is not to critique every single
study published on this subject, but rather to explain the proposed mechanism
for the drug interaction and then to highlight some of the issues with its
interpretation in relation to the medical literature.
What
happens during normal platelet aggregation?
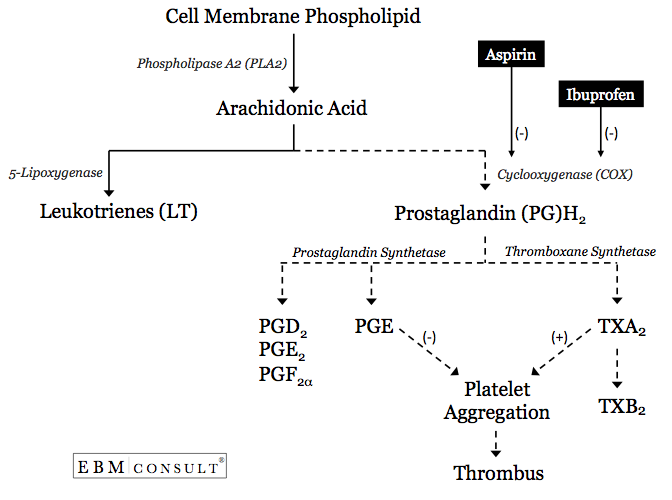
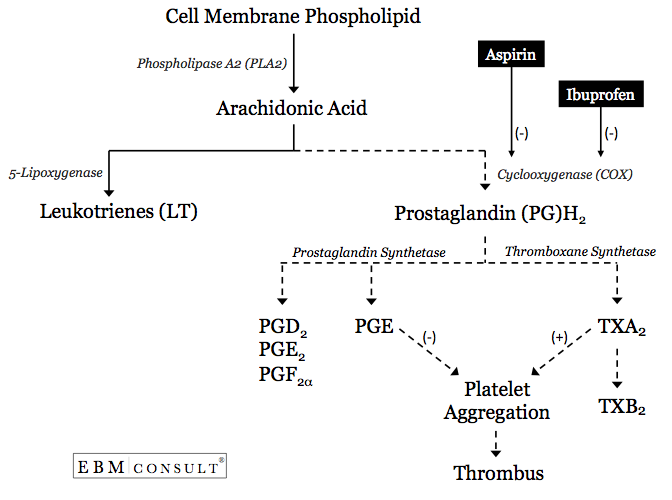
- The process of increased platelet aggregation begins with
the release of arachidonic acid (AA) from the cell membrane of a
platelet.6
- The AA can then goes down one of two metabolic pathways, the
lipoxygenase pathway, which will generate leukotrienes (LT), or the
cyclooxygenase (COX)-1 pathway to form prostaglandin (PG) H2.9 Prostaglandin H2 can then be metabolized by prostaglandin
synthetase to form other PGs or it can be metabolized by thromboxane (TX)
synthetase to form TXA2.
- If TXA2 is formed then platelet aggregation will
be facilitated or encouraged.10 This specifically occurs when AA is able
to travel through a hydrophobic channel where it can make contact with
catalytic site within the COX-1 enzyme. If this channel or the area
surrounding the catalytic site is blocked, the AA will be unable to be
metabolized to PGH2 and then onto TXA2, thereby reducing the likelihood for
platelet aggregation.6,9,11
How
does aspirin then interfere with platelet aggregation?
- Upon administration of aspirin, it will irreversibly
acetylate a serine residue at position 529 within the hydrophobic channel,
which is in close proximity to the catalytic site where AA can be metabolize to
platelet derived TXA2 by COX-1 enzyme.6,9,11 The acetylation of this area
creates a blockade where AA will not be able to gain access to the catalytic
site within COX-1.
- Since aspirin does this irreversibly, the ability of
that catalytic site within COX-1 enzyme to metabolize AA is blocked or
inhibited for the life of that platelet (usually around 7-12 days). This
is one of the main reasons aspirin confers a cardioprotective benefit against
cardiovascular events when primarily being used for secondary prevention.
- Therefore, if anything else competes or blocks aspirin's access to acetylate
this serine residue within the COX-1 enzyme, the cardioprotective benefits may
be diminished.
How
does ibuprofen interfere with the pharmacologic activity of aspirin?
- As with all of the NSAIDs, ibuprofen is a reversible,
competitive inhibitor of the catalytic site for AA metabolism within the
hydrophobic channel of the COX-1 enzyme.7,12
- The presence of ibuprofen
within this hydrophobic channel competitively blocks the access of aspirin to
acetylate the serine residue that is in close proximity to the catalytic site
for AA.7,12,13
- The degree of inhibition of aspirin's access to exert its
pharmacologic effect by ibuprofen is going to be influenced by a number of
factors.
The
first and most obvious factor has to do with the order with which aspirin and
ibuprofen are administered in relation to each other. If the aspirin is
given first, it will gain access to irreversibly acetylate the serine residue
within the COX-1 enzyme. Remember, once aspirin has irreversibly
inhibited the COX-1 enzyme, the antiplatelet effect will continue to exist for
the life for that platelet. The next factor is the concentration of
ibuprofen present in relation to the time of co-administration of
aspirin. Since ibuprofen's inhibition is competitive, platelet
aggregation is not only influenced by the concentration of ibuprofen present,
but is also reversible in nature. Therefore, as the drug levels decrease
through elimination pathways, the amount of ibuprofen able to block aspirin's
access to its active site also decreases, especially given its short half-life
of 2-4 hours.14 This pharmacokinetic characteristic of ibuprofen is the
reason why it must re-dosed multiple times throughout the day, whereas aspirin
is only dosed once a day. Therefore, one can see why there is variation
in the findings from multiple studies published in the medical
literature. Thus the clinical impact of this drug interaction is
influenced by the order in which the two medications are administered, the dose
and formulation of aspirin used, the dose and frequency of administration of
ibuprofen used, the patient population studied, and the type of endpoint from
that study.
In
the end, the real question is whether this interaction translates into a clinically
relevant pre-defined patient oriented cardiovascular defined outcome. To
our knowledge no such prospective, appropriately designed clinical trial has
been done to answer this question with convincing data in the population of
patients in question.
References:
- Gengo
FM, Rubin L, Robson M et al. Effects of ibuprofen on the magnitude and
duration of aspirin's inhibition of platelet aggregation: clinical consequences
in stroke prophylaxis. J Clin Pharmacol 2008;48:117-22.
- Gladding
PA, Webster MWI, Farrell HB et al. The antiplatelet effect of six
non-steroidal anti-inflammatory drugs and their pharmacodynamic interactions
with aspirin in healthy volunteers. Am J Cardiol
2008;101:1060-1063.
- Cryer
B, Berlin RG, Copper SA et al. Double-blind, randomized, parallel,
placebo-controlled study of ibuprofen effects on thromboxane B2 concentrations
in aspirin-treated healthy adult volunteers. Clin Ther
2005;27:185-191.
- MacDonald
TM, Wei L et al. Effect of ibuprofen on cardioprotective effect of
aspirin. Lancet 2003;361:573-74.
- Kurth
T, Glynn RJ, Walker AM et al. Inhibition of clinical benefits of aspirin
on first myocardial infarction by nonsteroidal antiinflammatory drugs.
Circulation 2003;108:1191-1195.
- Catella-Lawson
F, Reilly MP, Kapoor SC et al. Cyclooxygenase inhibitors and the
antiplatelet effects of aspirin. N Engl J Med
2001;345:1809-17.
- Evans
AM. Pharmacodynamics and pharmacokinetics of the profens:
enantioselectivity, clinical implications, and special reference to
S(+)-ibuprofen. J Clin Pharmacol 1996;36:7S-15S.
- Food
& Drug Administration. Information for healthcare professionals:
concomitant use of ibuprofen and aspirin. U.S. Department of Health &
Human Services. Last accessed: 09-19-2011.
- Funk
CD, Funk LB, Kennedy ME et al. Human platelet/erythroleukemia cell
prostaglandin G/H synthase: cDNA cloning, expression, and gene chromosomal
assignment. FASEB J 1991;5:2304-12.
- Fitzgerald
GA. Mechanisms of platelet activation: thromboxane A2 as an amplifying
signal for other agonists. Am J Cardiol 1991;68:11B-15B.
- Loll
PJ, Picot D, Garavito RM. The structural basis of aspirin activity
inferred from the crystal structure of inactivated prostaglandin H2
synthase. Nat Struct Biol 1995;2:637-43.
- Loll
PJ, Picot D, Ekabo O et al. Synthesis and use of iodinated nonsteroidal
antiinflammatory drug analogs as crystallographic probes of the prostaglandin
H2 synthase cyclooxygenase active site. Biochemistry
1996;35:7330-40.
- Rao
GH, Johnson GG, Reddy KR et al. Ibuprofen protects platelet
cyclooxygenase from irreversible inhibition by aspirin.
Arteriosclerosis 1983;3:383-8.