Procedure: Lumbar Puncture
Summary:
- Assuming the patient has no contraindications and the patient has given consent (assuming it is not an emergency), the following information will describe the steps involved to complete a lumbar puncture for the purpose of measuring the opening pressure and/or obtaining cerebrospinal fluid (CSF).
- To review the evidence on who should get a head CT prior to a lumbar puncture (LP) when evaluating for meningitis click here
Procedure: Lumbar Puncture; LP
|
|---|
- Presences of increased intracranial pressure (ICP), regardless of cause, can increase risk of cerebral or cerebellar brainstem herniation at the level of the foramen magnum.
- Use of anticoagulants (e.g., warfarin, enoxaparin, etc) due to increased risk of developing an epidural hematoma.
- Evidence of cellulitis or abscess over the area where LP would be performed due to risk of introducing infection into the subarachnoid space.
- Significant degenerative joint disease or prior back surgeries where hardware maybe in place (Note: many of these patients may require an LP under fluoroscopy)
- Herniation of the brainstem
- Accidental puncture of the aorta or vena cava leading to retroperitoneal hematoma
- Accidental puncture of the spinal cord from being in wrong location
- Infection being introduced into the subarachnoid space
- Pain over the LP site
- Headache
from CSF leak
- Can worsen with sitting up or standing, and if lasting longer than 1-2 days may require a blood patch in the area of the LP puncture site
- Verify that no contraindications exist.
- This may include doing a CT head to rule out active bleeding, midline shift, space-occupying lesions or signs of brain swelling.
- EBM Topic: Who needs a head CT prior to LP when evaluating for the presence of meningitis ...click here
- Explain the procedure to the patient and answer all questions
- Obtain informed consent with appropriate documentation
- Do a baseline neurologic exam with special notation on the strength, sensation and ability to move extremities
- Place the necessary orders so that the CSF tubes can be labeled after the procedure is completed
- Wash hands, open the lumbar puncture tray without compromising sterility and consider any extra supplies (i.e., spinal needles or extra tubes)
- Position the patient either in lateral decubitus / fetal position, or sitting upright leaning forward over a small table
- Opening pressures cannot be obtained accurately if the patient is upright.
- If opening pressures are indicated, the patient will need to straighten out after insertion of the needle to accurately measure the opening and closing pressure, because they can be falsely increased with the pressure applied to the abdomen in a fetal position
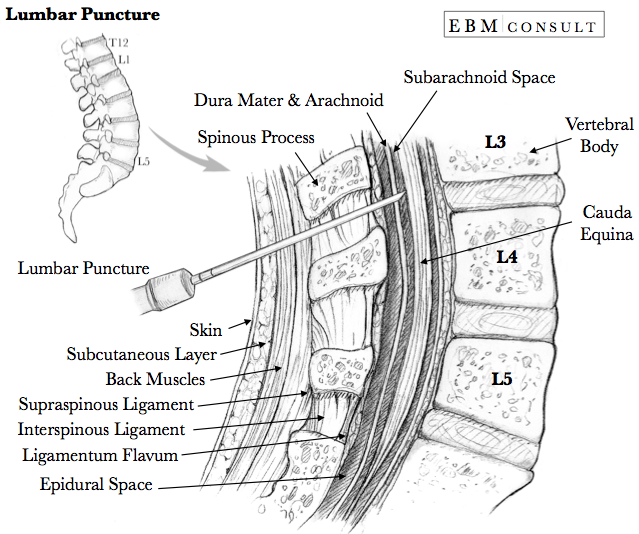
- Locate the L3/L4 space by locating the superior iliac crests and placing your thumbs midline to the spine. Palpate above and below to determine the widest space and attempt to mark location with the nail of your thumb or create a small indentation with an object like pen or needle cap
- Aseptically clean the skin using chlorhexidine skin prep
- Some clinicians will do this using the skin prep provided in the LP tray once they have their sterile gloves on
- EBM Focused Topic: Chlorhexidine vs. povidone-iodine (Betadine) in invasive procedures ... click here
- Put on sterile gloves, facemask, and protective gear per institutional policy
- Finish setting the LP tray including opening the CSF tubes in preparation to be easily accessed, and apply the sterile drapes to the patient
- Draw up and inject 10 mL of 1% or 2% lidocaine (preservative free; without epinephrine) to the area
- Consider injecting some anesthetic a level above or below this area in case an adjustment is needed
- Insert
the spinal needle directed at a slight cephalad angle (imagine aiming towards the umbilicus) and with the
bevel of the needle oriented to the longitudinal fibers in attempt to separate the fibers instead of cutting them
- If the patient is lying in lateral decubitus position the bevel should be oriented up
- If the patient is sitting upright and leaning forward the bevel should be oriented to the left or right
- The entry into the subarachnoid space is commonly described as feeling a "pop" sensation, the needle insert (obturator) is then removed and CSF should begin to drip out
- Have the patient slowly stretch out legs (if lying in lateral decubitus)
- Attach the sterile manometer to the end of the spinal needle to measure the opening pressure
- Normal opening pressures: < 20 cm H2O
- Measuring opening pressure is very important for evaluation for cryptococcal meningitis or pseudotumor cerebri
- If blockage of CSF flow to the spinal subarachnoid space is suspected, the clinician may perform a Queckenstedt-Stookey test
- Empty the manometer into CSF tube #1 and about 10 drops of CSF into tubes #2 - 4 (note: some institutions use only 3 tubes)
- Measure the closing pressure (if indicated)
- Reinsert the needle insert (obturator) and withdraw the spinal needle and immediately apply pressure and an adhesive bandage over the insertion site
- While the traditional teaching is to have the patient remain lying flat after a procedure, there is no evidence that it has any effect on the development of post-LP headache. At the same time, there is no harm in having the patient lie flat if they desire to do so.
- Despite the lack of evidence, some clinicians will have the patient lay prone with a pillow under the abdomen to increase the pressure on the tissues around the area of the LP in the thought that it might prevent CSF leaking.
- While based on expert opinion only, some clinicians will encourage and counsel the patient to drink extra fluids to help replace the CSF drained off and prevent a headache (or give the patient IV fluids if warranted)
- Immediately label the CSF tubes have the tubes hand carried/delivered to the lab for analysis
- If meningitis is suspected, initiate empiric antibiotics with or without steroids based on the clinical scenario
- Repeat neurologic assessment to evaluate for any changes post-LP
- Document the procedure, number of attempts, opening and closing pressure (if applicable), total amount of CSF drained
- Before the procedure, no fasting needed
- During
the procedure, encourage the patient to not move and try to remain calm
- After the procedure, encourage fluid intake to prevent headache and consider resting and lying flat for first 12 hours to help prevent possible headaches while things heal
- EBM Focused Topic: Risk Factors for Brain Stem Herniation When Doing a Lumbar Puncture
- EBM Focused Topic: Chlorhexidine vs. Povidone-Iodine for Prevent Post-Procedure and Surgical Infections
- EBM Focused Topic: Nimodipine Use for Subarachnoid Hemorrhage
- Anatomy: Cavernous Sinus
- Anatomy: Homunculus (Motor & Sensory)
- Anatomy & Pathology: Subdural vs. Epidural Hematoma
Contraindications
Complications
The following are in order of most concerning to the least:
Before the Procedure
During the Procedure
After the Procedure
Counseling Points
Related Content
To see other related content please click or tap on an item: