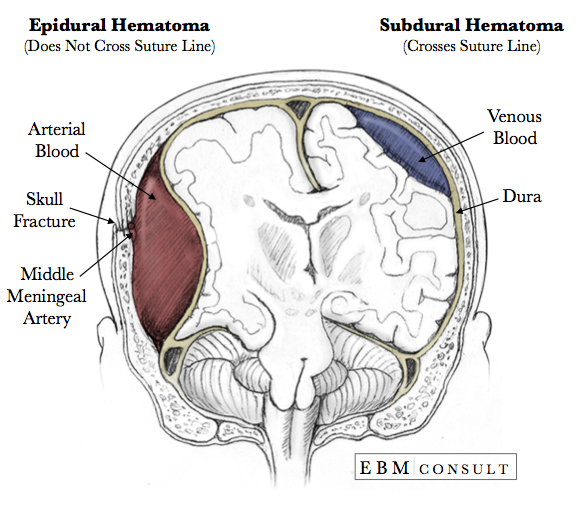
Anatomy: Epidural vs. Subdural Hematoma
|
|---|
- Epidural hematomas occur when an artery is injured and arterial blood accumulates between the dura and the calvarium.
- Do not cross suture lines because of the tight adherence of the dura to the calvarium and thus have a biconvex or elliptical appearance.
- The middle meningeal artery is classically involved, especially with a skull fracture.
- Associated with a "lucid interval", which means that a patient can be conscious and appear "normal" right after an injury, but as the blood accumulates the headache will worsen and mental status will decline as the intracranial pressure rises.
- Tearing of bridging veins during rapid or sudden changes in velocity thereby causing an accumulation of venous blood below the dura but above the arachnoid membrane (i.e., the "subural space").
- Cross suture lines since bleeding is below the dura, which is tightly attached to the calvarium, thus giving the "crescent shape" appearance on head CT.
- Can result in mass effect leading to uncal and/or tonsillar herniation if left untreated.
- Occur more frequently in elderly patients due to reduced brain volume and "stretched" bridging veins.
- General Info: Caused by increased intracranial pressure (ICP) which can lead to 4 types of herniation: central, subfalcine, tonsillar, and uncal (or transtenorial) herniation
- Pathophysiology: As the ICP increases, the CSF is initially forced to move down into the spinal canal and then the ventricles and cisterns begin to collapse. It is at this point that the ICP can rise rapidly resulting in a shift of the brain parenchyma away from the accumulating blood. If swelling progresses, the parenchyma will have to shift through several different spaces with the final movement being through the foramen magnum causing compression of the brainstem and death.
- If no contraindications exist (such as thoracic or lumbar spine injury without stabilization), raise the head of the bed to 30 degrees, keep head and neck midline, and avoid tight fitting cervical collars unless medically necessary
- If the head of the bed is contraindicated due to other injuries, place patient in reverse Trendelenburg (i.e., elevate the entire the bed up higher from the ground and then lower portion of the bed where the legs are so that the head is higher than the level of the heart).
- Note: Do not use if patient is hypotensive and/or hypovolemic as it can decrease blood pressure and thus reduce cerebral perfusion pressure (CPP).
- 0.5 - 1.0 mg/kg IV over 15 minutes
- Works to reduce cerebral edema by creating an osmotic gradient between the vascular space and the extracellular fluid of the brain, thereby causing water to shift out of the brain into the vascular space to reduce brain volume and ICP.
- 3% NaCl = 200 mL IV over 20 min
- 7.2% - 7.5% NaCl = 1.5 - 2 mL/kg IV over 15-20 minutes, respectively
- 23.4% NaCl = 30 mL IV over 2 min or over 30 min when the ICP is > 20 mm Hg
- Note! Only for short-term use in patients with evidence of brain herniation to prepare for surgical intervention as reducing the PCO2 to ≤ 25 mm Hg can significantly reduce cerebral blood flow and oxygen delivery.
- Moderate short-term hyperventilation to PCO2 of no less than 30 - 35 mm Hg
- Pentobarbital = Loading dose of 10 mg/kg IV over 30 min, followed by 5 mg/kg/hr IV x 3 hrs, then 1 mg/kg/hr and adjust dose to maintain suppression of bursts on continuous EEG
- Etomidate = 0.2 mg/kg IV x 1 then 0.05 mg/kg every 3-5 min as needed (can decrease ICP without affecting cardiac output or blood pressure, but has potential to suppress adrenal function)
- Fosphenytoin (Cerebyx) = Loading dose of 10 - 20 PE/kg IV x 1 (administer at max rate of 150 mg/min IV push), then 4 - 6 mg/kg/day in 2 - 3 divided doses x 7 days
- Phenytoin (Dilantin) = Loading dose of 10 - 20 mg/kg IV x 1 (give at max rate of no more than 50 mg/min IV push due to risk of bradydysrhythmias and hypotension), then 100 mg IV every 8 hrs x 7 days
- Levetiracetam (Keppra) = 1000 mg (or 20 mg/kg rounded to the nearest 250 mg) IV over 15 min, then 1000 - 2000 mg IV every 12 hrs x 7 days
- Invasive removal of CSF by a neurosurgeonis one of the most effective treatments for lowering ICP
- Maintain normovolemia so that the patient does not develop hypotension which can reduce cerebral perfusion pressure. Note: avoid use of hypotonic fluids as this will encourage movement of free water into the brain tissue and worsen swelling.
- This controversial with conflicting data and thus is not universally recommended. It is important however to prevent and/or treat fevers.
- EBM Topic: The Evidence for the HINTS Exam in the Bedside Diagnosis of Central Causes of Dizziness
- EBM Topic: The Evidence for Endovascular Therapy in Acute Stroke
- EBM Topic: The Evidence for Nimodipine Use for Subarachnoid Hemorrhage
- Anatomy Image: Bells Palsy vs Stroke
- Anatomy Image: Dermatomes - Full Body
- Anatomy Image: Dermatomes - Face
- Anatomy Image: Dermatomes - Hands
- Procedure: Lumbar Puncture
- Schwartz ML, et al. The University of Toronto head injury treatment study: A prospective randomised comparison of pentobarbital and mannitol. Can J Neurol Sci 1984;11:434-440.
- Muizelaar JP, et al. Effect of mannitol on ICP and CBF and correlation with pressure autoregulation in severely head injured patients. J Neurosurg 1984;61:700-706.
- Mendelow AD, et al. Effect of mannitol on cerebral blood flow and cerebral perfusion pressure in human head injury. J Neurosurg 1985;63:43-48.
- Smith HP, et al. Comparison of mannitol regimens in patients with severe head injury undergoing intracranial monitoring. J Neurosurg 1986;65:820-824.
- Rosner MJ, et al. Cerebral perfusion pressure: a hemodynamic mechanism of mannitol and the pre-mannitol hemogram. Neurosurg 1987;21:147-156.
- Cruz J, et al. Continuous monitoring of cerebral oxygenation in acute brain injury: injection of mannitol during hyperventilation. J Neurosurg 1990;73:725-730.
- Cruz J et al. Improving clinical outcomes from acute subdural hematomas with emergency preoperative administration of high doses of mannitol: a randomized trial. Neurosurgery 2001;49(4):864-71.
- Cruz J et al. Major clinical and physiological benefits of early high doses of mannitol for intraparenchymal temporal lobe hemorrhages with abnormal pupillary widening: a randomized trial. Neurosurgery 2002;51(3):628-38.
- Cruz J et al. Successful use of the new high-dose mannitol treatment in patients with Glascow Coma Scale Scores of 3 and bilateral abnormal pupillary widening: a randomized trial. J Neurosurg 2004;100(3):376-83.
- Wisner JD, et al. Hypertonic saline resuscitation of head injury: effects on cerebral water content. J Trauma 1990;30:75-78.
- Vassar MJ, et al. 7.5% sodium chloride/dextran for resuscitation of trauma patients undergoing helicopter transport. Arch Surg 1991;126:1065-1072.
- Mattox KL, et al. Prehospital hypertonic saline/dextran infusion for post-traumatic hypotension. Ann Surg 1991;213:482-491.
- Schmoker JD, et al. Hypertonic fluid resuscitation improves cerebral oxygen delivery and reduces intracranial pressure after hemorrhagic shock. J Trauma 1991;31:1607-1613.
- Prough DS, et al. Rebound intracranial hypertension in dogs after resuscitation with hypertonic solutions from hemorrhagic shock accompanied by an intracranial mass lesion. J Neurosurg Anesthesiol 1999;11:102-11.
- Munar F et al. Cerebral hemodynamic effects of 7.2% hypertonic saline in patients with head injury and raised intracranial pressure. J Neurotrauma 2000;17(1):41-51.
- Vialet R et al. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 ml/kg 7.5% saline is more effective than 2 ml/kg 20% mannitol. Crit Care Med 2003;31(6):1683-7.
- Huang SJ et al. Efficacy and safety of hypertonic saline solutions in the treatment of severe head injury. Surg Neurol 2006;65(6):539-46.
- Kerwin AJ et al. The use of 23.4% hypertonic saline for the management of elevated intracranial pressure in patients with severe traumatic brain injury: a pilot study. J Trauma 2009;67(2):277-82.
- Paul RL, et al. Intracranial pressure responses to alterations in arterial carbon dioxide pressure in patients with head injuries. J Neurosurg 1972;36:714-720.
- Obrist WD, et al. Cerebral blood flow and metabolism in comatose patients with acute head injury. J Neurosurg 1984;61:241-253.
- Muizelaar JP, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: A randomized clinical trial. J Neurosurg 1991;75:731-739.
- Sheinberg M, et al. Continuous monitoring of jugular venous oxygen saturation in head injured patients. J Neurosurg 1992;76:212-217.
- Gopinath SP, et al. Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psych 1994;57:717-723.
- Inaba K et al. A prospective multicenter comparison of levetiracetam vs phenytoin for early posttraumatic seizure prophylaxis. J Trauma Acute Care Surg. 2013;74(3):766-71.
- Szaflarski JP et al. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care. 2010;12(2):165-72.
- Jones KE et al. Levetiracetam versus phenytoin for seizure prophylaxis in severe traumatic brain injury. Neurosurg Focus. 2008;25(4): E3.
- Zafar SN et al. Phenytoin versus Levetiracetam for seizure prophylaxis after brain injury - a meta analysis. BMC Neurol. 2012;12:30.
Epidural Hematoma
Subdural Hematoma
Brain Herniation
Treatments
The goal for considering any one or more of the following is to maintain cerebral perfusion pressure and to reduce metabolic demands by avoiding secondary injury to the CNS.
Elevation of the Head
Mannitol
Hypertonic Saline
Hyperventilation
Barbiturates or Sedatives
Anticonvulsants
Mainly for patients with traumatic brain injury, especially penetrating injuries and/or depressed skull fractures.
Ventriculostomy
IV Fluids
Therapeutic Hypothermia
Related Content
References
Mannitol
Hypertonic Saline
Hyperventilation
Anticonvulsants