Rifaximin (Xifaxan): Drug Monograph
|
|---|
- Reduction in risk of overt hepatic encephalopathy (HE) recurrence in adults
- Treatment of irritable bowel syndrome with diarrhea (IBS-D) in adults
- Treatment of travelers' diarrhea caused by noninvasive strains of Escherichia coli in adults and pediatric patients ≥12 years of age
- General Notes: Take with or without food
- Hepatic encephalopathy:
- 550 mg by mouth twice daily
- Note: Other unapproved doses that have been used in practice: 400 mg every 8 hours x 5-10 days
- Irritable bowel syndrome with predominance of diarrhea (IBS-D):
- 550 mg by mouth three times a day x 14 days
- May retreat up to two times with the same dosage regimen in patients who have recurrence of symptoms
- Traveler's diarrhea:
- 200 mg by mouth three times a day x 3 days
- Travelers' diarrhea, ≥12 years:
- 200 mg by mouth three times a day x 3 days
- History of hypersensitivity to rifaximin, rifamycin antimicrobial agents, or any of the components of the drug
- Traveler's diarrhea not caused by E. coli - rifaximin is not effective in diarrhea complicated by fever and/or blood in the stool or diarrhea due to pathogens other than E. coli. If diarrhea symptoms get worse or persist for more than 24 to 48 hours discontinue treatment and consider alternative antibiotics
- Clostridium difficile-associated diarrhea - evaluate if diarrhea occurs after therapy or does not improve or worsens during therapy
- Use with caution in patients with severe (Child-Pugh Class C) hepatic impairment
- Concomitant use of rifaximin and a P-glycoprotein inhibitor - exercise caution
- Increased risk of the development of drug-resistant bacteria if rifaximin is used for travelers' diarrhea in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication
- No specific information available on the treatment
- Discontinue the drug, treat symptomatically, and institute supportive measures as required
- Cytochrome P450 enzymes:
- CYP3A4 substrate
- Drug Interaction Considerations:
- Cyclosporine - significantly increases the systemic exposure to rifaximin
- Pregnancy: Pregnancy Category Unknown. Advise pregnant women of the potential risk to a fetus
- Labor and Delivery: None
- Nursing Mothers: No information regarding the presence of rifaximin in human milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production. Consider the benefits and risk to nursing mothers.
- Renal Impairment: None
- Hepatic Impairment: None
- Pediatric Patients: The safety and effectiveness has not been established in patients <12 years of age with Traveler's diarrhea or in patients <18 years of age for hepatic encephalopathy and IBS-D.
- Geriatric Patients: No overall differences in safety or effectiveness observed between older and younger subjects with HE and IBS-D. Greater sensitivity of some older individuals cannot be ruled out.
- No information regarding the presence of rifaximin in human milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production. Consider the benefits and risk to nursing mothers.
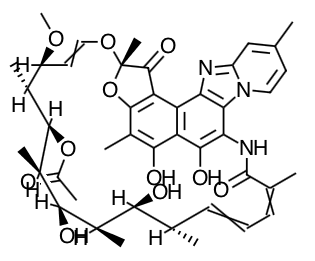
- Scientific Name: (2S,16Z,18E,20S,21S,22R,23R,24R,25S,26S,27S,28E)-5,6,21,23,25- pentahydroxy-27-methoxy-2,4,11,16,20,22,24,26-octamethyl-2,7-(epoxypentadeca-[1,11,13] trienimino)benzofuro[4,5-e]pyrido[1,2-á]-benzimidazole-1,15(2H)-dione,25-acetate
- Empirical Formula: C43H51N3O11
- Molecular Weight: 785.9
- Rifaximin is an antibacterial drug that is reported to inhibit bacterial DNA-dependent RNA and polymerase thereby resulting in inhibition of bacterial protein synthesis and consequently inhibition of the growth of bacteria.
- Absorption: Limited except for patient with hepatic encephalopathy where the mean rifaximin exposure (AUC) was approximately 12- fold higher than that observed in healthy subjects.
- Distribution: In vivo, the mean protein-binding ratio was 67.5% in healthy subjects and 62% in patients with hepatic impairment when rifaximin was administered.
- Metabolism: In an in vitro study, rifaximin was metabolized mainly by CYP3A4.
- Elimination: The mean half-life of rifaximin in healthy subjects at steady state was 5.6 hours and was 6 hours in IBS-D patients.
- Specific Populations
- Hepatic Impairment: The mean AUC in patients with hepatic impairment of Child-Pugh Class A, B, and C was 10-, 14-, and 21-fold higher, respectively, compared to that in healthy subjects.
- Renal Impairment: The pharmacokinetics in patients with impaired renal function have not been studied.
- Drug Interactions
- Cyclosporine: In vitro in the presence of P-glycoprotein inhibitor, verapamil, the efflux ratio of rifaximin was reduced greater than 50%. In a clinical drug interaction study, mean Cmax for rifaximin was increased 83-fold, from 0.48 to 40.0 ng/mL; mean AUC∞ was increased 124-fold, from 2.54 to 314 ng•h/mL following co-administration of a single dose of rifaximin 550 mg with a single 600 mg dose of cyclosporine, an inhibitor of P-glycoprotein. Cyclosporine is also an inhibitor of OATP, breast cancer resistance protein (BCRP) and a weak inhibitor of CYP3A4. The relative contribution of inhibition of each transporter by cyclosporine to the increase in rifaximin exposure is unknown.
- Effect of rifaximin on other drugs: In in vitro drug interaction studies the IC50 values for rifaximin was >50 micromolar (~60 mcg) for CYP isoforms 1A2, 2A6, 2B6, 2C9, 2C19, 2D6, and 2E1. In vitro IC50 value of rifaximin for CYP3A4 was 25 micromolar. Based on in vitro studies, clinically significant drug interaction via inhibition of 1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1 and 3A4 by rifaximin is not expected. The inhibitory effect of rifaximin on P-glycoprotein transport was observed in an in vitro study. The effect of rifaximin on P-gp transporter was not evaluated in vivo. In in vitro studies, rifaximin at 3 micromolar inhibited the uptake of estradiol glucuronide via OATP1B1 by 64% and via OATP1B3 by 70% while the uptake of estrone sulfate via OATP1A2 was inhibited by 40%. The inhibitory potential of rifaximin on these transporters at the clinically relevant concentrations is unknown.
- Midazolam: In an in vitro study, rifaximin was shown to induce CYP3A4 at the concentration of 0.2 micromolar. No significant induction of CYP3A4 enzyme using midazolam as a substrate was observed when rifaximin was administered three times a day for 7 days at 200 mg and 550 mg doses in two clinical drug interaction studies in healthy subjects. The effect of 200 mg administered orally every 8 hours for 3 days and for 7 days on the pharmacokinetics of a single dose of either 2 mg intravenous midazolam or 6 mg oral midazolam was evaluated in healthy subjects. No significant difference was observed in the systemic exposure or elimination of intravenous or oral midazolam or its major metabolite, 1'-hydroxymidazolam, between midazolam alone or together with rifaximin. Therefore, rifaximin was not shown to significantly affect intestinal or hepatic CYP3A4 activity for the 200 mg three times a day dosing regimen. When single dose of 2 mg midazolam was orally administered after administration of rifaximin 550 mg three times a day for 7 days and 14 days to healthy subjects, the mean AUC of midazolam was 3.8% and 8.8% lower, respectively, than when midazolam was administered alone. The mean Cmax of midazolam was lower by 4 to 5% when rifaximin was administered for 7-14 days prior to midazolam administration. This degree of interaction is not considered clinically meaningful.
- Oral Contraceptives Containing Ethinyl Estradiol and Norgestimate: The oral contraceptive study utilized an open-label, crossover design in 28 healthy female subjects to determine if rifaximin 200 mg orally administered three times a day for 3 days (the dosing regimen for travelers' diarrhea) altered the pharmacokinetics of a single dose of an oral contraceptive containing 0.07 mg ethinyl estradiol and 0.5 mg norgestimate. Results showed that the pharmacokinetics of single doses of ethinyl estradiol and norgestimate were not altered by rifaximin. An open-label oral contraceptive study was conducted in 39 healthy female subjects to determine if rifaximin 550 mg orally administered three times a day for 7 days altered the pharmacokinetics of a single dose of an oral contraceptive containing 0.025 mg of ethinyl estradiol (EE) and 0.25 mg norgestimate (NGM). Mean Cmax of EE and NGM was lower by 25% and 13%, after the 7-day rifaximin regimen than when the oral contraceptive was given alone. The mean AUC values of NGM active metabolites were lower by 7% to approximately 11%, while AUC of EE was not altered in presence of rifaximin. The clinical relevance of the Cmax and AUC reductions in the presence of rifaximin is not known.
- Advise patients being treated for travelers' diarrhea to discontinue treatment if diarrhea persists more than 24-48 hours or worsens. Advise the patient to seek medical care for fever and/or blood in the stool.
- Advise patients that they can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If diarrhea occurs after therapy or does not improve or worsens during therapy, advise patients to contact a physician as soon as possible.
- Advise patients that rifaximin should only be used to treat bacterial infections not viral infections (e.g., the common cold). The medicine should be taken exactly as directed. Skipping doses or not completing the full course of therapy may decrease the effectiveness of the immediate treatment and increase the likelihood that bacteria will develop resistance and will not be treatable by rifaximin or other antibacterial drugs in the future.
- Inform patients with severe hepatic impairment (Child-Pugh Class C) that there is an increase in systemic exposure to rifaximin.
- Pharmacology: The Mechanism and Cross-Reactivity in Penicillin and Cephalosporin Antibiotics
- Drug Monograph: Aztreonam (Azactam; Cayston)
- Drug Monograph: Ceftriaxone (Rocephin)
- Drug Monograph: Linezolid (Zyvox)
- Drug Monograph: Nitrofurantoin (Macrobid)
Indications
Dosing
(Adult)
(Pediatric)
Contraindications
Warnings
Overdose
Drug Interactions
Special Populations
Breastfeeding
Chemical Structure
Mechanism of Action
Pharmacokinetics
Counseling Points
Other EBM Consult Related Content
MESH Terms & Keywords
|
|---|
|

