-
The
use of herbal or natural medicines is increasing among patients and many of
these products share pharmacologic properties with medications that require a
prescription.1 It is also well known that oral antiplatelet medications
(such as aspirin, clopidogrel, prasugrel, ticlopidine, dipyridamole/aspirin)
for the prevention and/or treatment of cardiovascular diseases (CVD) and oral
anticoagulants, such as warfarin, for the prevention and/or treatment of
thrombotic related disorders are common across the world. This risk for
bleeding due to antiplatelet effects can also be increased with the use of
non-steroidal anti-inflammatory drugs (NSAIDs). Their use may be initiated
by a healthcare provider or by patients themselves since they can purchase them
over-the-counter (OTC) for any pain related problems. In fact, the use of
self-initiated NSAIDs is fairly common. According to a survey of 4,263
people in 2002 by the National Consumer League, ibuprofen was the most common
OTC medication at 38% of consumers followed by acetaminophen at 33%, aspirin at
16% and naproxen at 9%.2 While in some cases the coadministration of two
or more antiplatelet drugs may be medically necessary, use of any of these
drugs incurs risk and this risk is compounded when multiple agents are
employed. Therefore, whether intentional or not, the concomitant use of
medications that are known to have antiplatelet effects can could put the
patient at additional risk for bleeding, especially if they are already taking
an anticoagulant.
Unfortunately,
the use of herbal or natural medicines may contribute to these effects without
the knowledge of the healthcare provider caring for that patient. As
such, a thorough medication use evaluation should be performed for the purposes
of identifying herbal products that may have been initiated by the patient
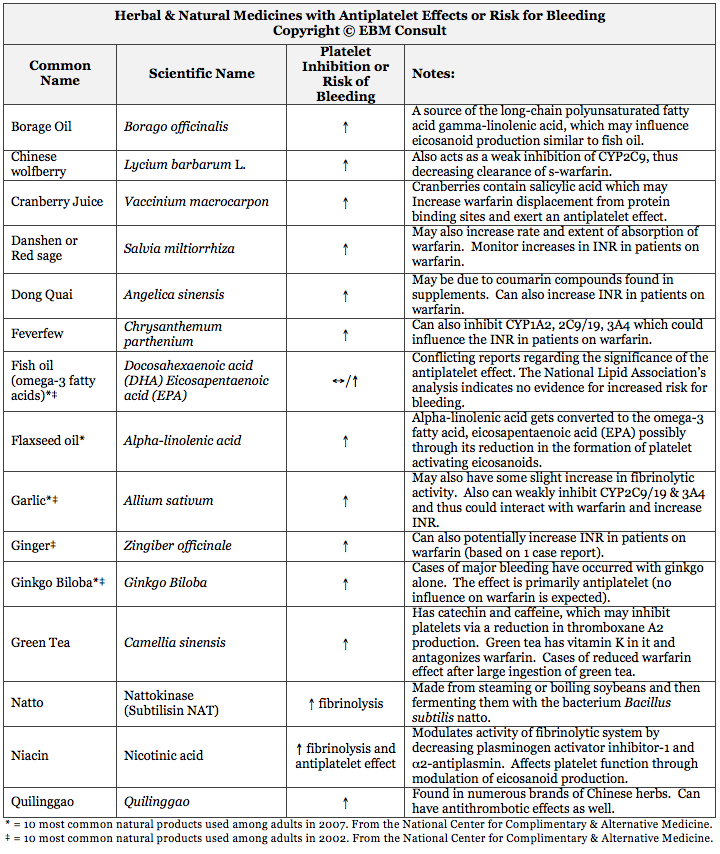
without the knowledge of the clinician. The table below provides a
summary of commonly used herbal and natural medicines that are known to have
either antiplatelet properties or to increase the risk of bleeding through
other mechanisms known to influence hemostasis.3-26
It
is also important for clinicians to recognize that while many of these herbal
products can inhibit platelet aggregation or hemostasis, some of them can also
increase the international normalized ratio (INR) in patients taking
warfarin. This could obviously put the patient at even greater risk
for clinically relevant bleeding. Of note, there is wide spread belief
that fish oil supplements (omega-3 fatty acids) put the patient at increased
risk for bleeding. The National Lipid Association did a thorough
evaluation of the available data and did not find any significant evidence that
fish oil supplements confer this effect.12 However, in patients with
active or uncontrolled bleeding it would still be prudent to hold the fish oil
supplement just in case.12
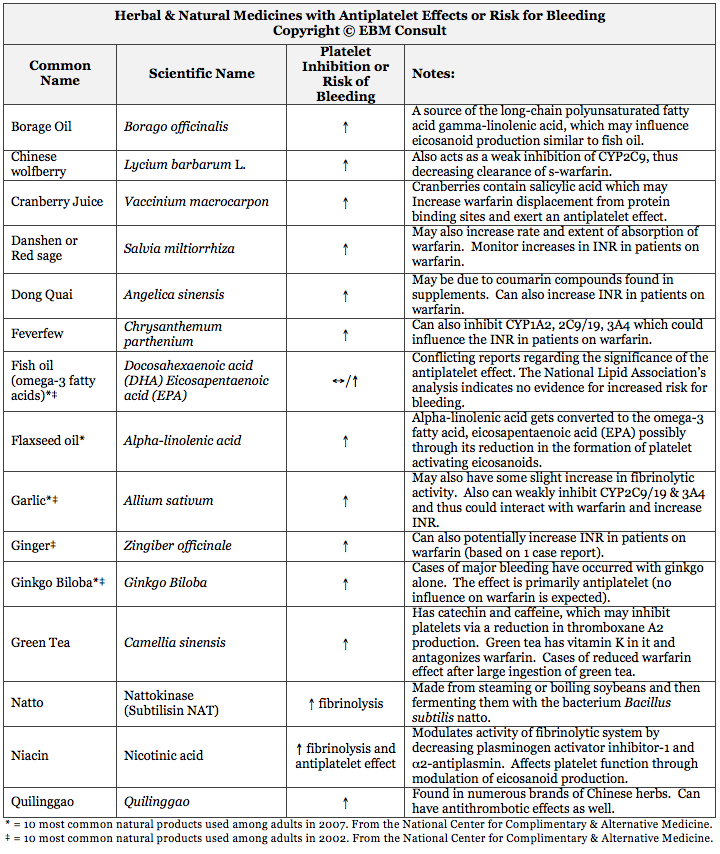
Based
on the table, it is evident that there are many common herbal products that
have been shown to have antiplatelet properties and/or influence
hemostasis. EBM Consult hopes that this table provides a user
friendly summary of those herbal and natural medicines that may be encountered
in clinical practice.
References:
- National Center for Complementary and Alternative Medicine: National
Institutes of Health. The Use of complementary and alternative medicine
in the United States: 2007 National Health Interview Survey Report.
Last accessed on 1-17-2009.
- Wilcox
CM, Cryer B, Triadafilopoulos G. Patterns of use and public perception
of over-the-counter pain relievers: focus on nonsteroidal
anti-inflammatory drugs. J Rheumatol 2005;32:2218-24.
- Lam
AY, Elmer GW, Mohutsky MA. Possible interaction between warfarin and
Lycium barbarum L. Ann Pharmacother 2001;35:1199-201.
- Leung
H, Hung A, Hui AC et al. Warfarin overdose due to the possible effects
of Lycium barbarum L. Food Chem Toxicol 2008;46:1860-2.
- Suvarna R, Pirmohamed M, Henderson L. Possible interaction between warfarin and cranberry juice. BMJ 2003;327:1454.
- Rindone
JP, Murphy TW. Warfarin-cranberry juice interaction resulting in
profound hypoprothrombinemia and bleeding. Am J Ther 2006;13:283-4.
- Aston JL, Lodoice AE, Shapiro NL. Interaction between warfarin and cranberry juice. Pharmacotherapy 2006;26:1314-9.
- Duthie
GG, Kyle JA, Jenkinson AM et al. Increased salicylate concentrations
in urine of human volunteers after consumption of cranberry juice. J
Agric Food Chem 2005;53:2897-900.
- Chan
K, Lo AC, Yeung JH et al. The effects of Danshen (Salvia miltiorrhiza)
on warfarin pharmacodynamics and pharmacokinetics of warfarin
enantiomers in rats. J Pharm Pharmacol 1995;47:402-6.
- Chan TY. Interaction between warfarin and danshen (Salvia miltiorrhiza). Ann Pharmacother 2001;35:501-4.
- Page RL 2nd, Lawrence JD. Potentiation of warfarin by dong quai. Pharmacotherapy 1999;19:870-6.
- Bays HE. Safety considerations with omega-3 fatty acid therapy. Am J Cardiol 2007;99[suppl]:35C-43C.
- Hendler SS, Rorvik DM. Flaxseed oil. In: PDR for Nutritional Supplements. 2nd Ed. Physicians' Desk Reference Inc. Montvale, NJ. 2008:218-221.
- Cassileth BR, Lucarelli C. Garlic. In: Herb-Drug Interactions in Oncology. BC Decker Inc. Hamilton, Ontario. 2003:163-164.
- Foster
BC, Foster MS, Vandenhoek S et al. An in vitro evaluation of human
cytochrome P450 3A4 and P-glycoprotein inhibition by garlic. J Pharm
Pharm Sci 2001;4:176-84.
- Lesho EP, Saullo L, Udvari-Nagy S. A 76 year-old woman with erratic anticoagulation. Cleve Clin J Med 2004;71:651-6.
- Vale S. Subarachnoid haemorrhage associated with Ginkgo biloba. Lancet 1998;352:36.
- Engelsen
J, Nielsen JD, Hansen KF. [Effect of coenzyme Q10 and Ginkgo biloba on
warfarin dosage in patients on long-term warfarin treatment. A
randomized, double-blind, placebo-controlled cross-over trial]. Ugeskr
Laeger 2003;165:1868-71.
- Mohutsky
MA, Anderson GD, Miller JW et al. Ginkgo biloba: evaluation of CYP2C9
drug interactions in vitro and in vivo. Am J Ther 2006;13:24-31.
- Fujita
M, Nomura K, Hong K et al. Purification and characterization of a
strong fibrinolytic enzyme (nattokinase) in the vegetable cheese natto, a
popular soybean fermented food in Japan. Biochem Biophys Res Commun
1993;197:1340-7.
- Chang
YY, Liu JS, Lai SL et al. Cerebellar hemorrhage proviked by combined
use of nattokinase and aspirin in a patient with cerebral microbleeds.
Intern Med 2008;47:467-9.
- Suzuki
Y, Kondo K, Matsumoto Y et al. Dietary supplementation of fermented
soybean, natto, suppresses intimal thickening and modulates the lysis of
mural thrombi after endothelial injury in rat femoral artery. Life
Sci 2003;73:1289-98.
- Urano
T, Ihara H, Umemura K et al. The profibrinolytic enzyme subtilisin NAT
purified from Bacillus subtilis cleaves and inactivates plasminogen
activator inhibitor type 1. J Biol Chem 2001;276:24690-6.
- Johansson
JO, Egberg N, Asplund-Carlson A et al. Nicotinic acid treatment shifts
the fibrinolytic balance favourably and decreases plasma fibrinogen in
hypertriglyceridemic men. J Cardiovasc Risk 1997;4:165-71.
- Saareks
V, Mucha I, Sievi E et al. Nicotinic acid and pyridoxine modulate
arachidonic acid metabolism in vitro and ex vivo in man. Pharmacol
Toxicol 1999;84:274-80.
- Wong AL, Chan TY. Interaction between warfarin and the herbal product quilinggao. Ann Pharmacother 2003;37:836-8.
|